Nilotinib appears safe in Parkinson’s trial; drug thought to allow dopamine replenishment

A clinical trial investigating the repurposed cancer drug nilotinib in people with Parkinson’s disease finds that it is reasonably safe and well tolerated. Researchers also report finding an increase in dopamine, the chemical lost as a result of neuronal destruction, and a decrease in neurotoxic proteins in the brain among study participants. Finally, they say nilotinib, a tyrosine kinase inhibitor, potentially halts motor and non-motor decline.
The results of the small, phase II trial conducted at Georgetown University Medical Center (GUMC) are published Dec. 16 in JAMA Neurology.
“Determining the safety of nilotinib in people with Parkinson’s was our primary objective,” explains Georgetown neurology associate professor Charbel Moussa, MBBS, Ph.D., the senior author of the study, and director of the GUMC Translational Neurotherapeutics Program.
Seventy-five participants (average age 68.4) with moderately advanced (stage 2.5-3) Parkinson’s disease and stable symptoms participated in the trial. They were randomized to receive either placebo, 150mg or 300 mg of nilotinib. Twenty-five participants were in each group.
To prevent bias in reporting, the study was blinded, meaning neither the study participants nor the study investigators knew if the active drug or placebo were being administered until the end of the individual’s study period. Participants took the placebo/nilotinib by mouth for 12 months, followed by a 3-month period of taking no placebo/nilotinib (washout).
Eighty-eight percent (88%) of the participants completed the study; two participants withdrew from the placebo group, three withdrew from the 150mg group (one voluntarily, two for non-compliance), and four in the 300mg group withdrew (one voluntary, one due to non-compliance and two for significant adverse events).
Nilotinib (Tasigna by Novartis) is approved by the U.S. Food and Drug Administration (FDA) for the treatment of chronic myeloid leukemia. It carries an FDA “black-box warning” because of sudden death due to the inhibition of Abl tyrosine kinase, an important protein for cellular function. Nilotinib is administered in higher doses (300mg twice a day) for cancer treatment than were studied in this trial (150mg and 300 mgs once a day).
“Our study shows that at these lower doses, nilotinib does not seem to cause Abl inhibition, suggesting it shouldn’t have the same safety concerns that are potentially associated with Abl inhibition as might be the case at higher doses,” Moussa says. He adds that no one withdrew from the study due to tolerability.
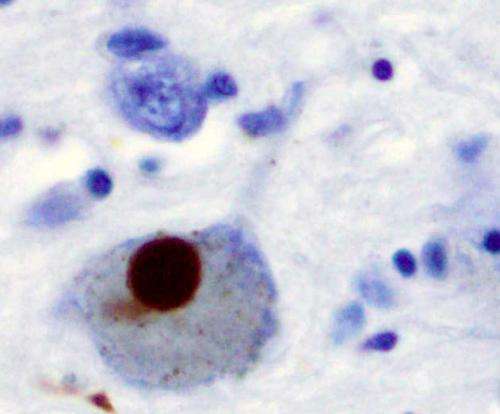
In a secondary finding of exploratory biomarkers, participants taking nilotinib had reduced levels of alpha-synuclein (20%) and tau (30%), two toxic proteins characteristic of those with Parkinson’s disease.
“Individually, these are very important findings, but taken together, it means that the clearance of these neurotoxic proteins may not solely depend on Abl inhibition—other tyrosine kinases or alternate mechanisms may be involved,” explains Moussa.
In addition, those taking nilotinib had a significantly increased level of dopamine metabolites (>50%) suggesting that the clearance of the toxic proteins allowed for an increased utilization of the brain’s own dopamine.
As part of the study, clinical outcomes were assessed at six, 12 and 15 months and compared to assessments at the start of the trial (baseline). Clinical testing was conducted at the optimal time of day for each participant based on the individual’s standard of care treatment (typically levodopa or a similar drug).
In exploratory clinical findings, non-motor, quality-of-life self-reports (PDQ-39) appeared to worsen in the placebo group, but nilotinib appeared to mitigate this progression for at least 12 months.
In another clinical observation, all study groups seem to improve on motor testing (UPDRS-III) at six months, however, those on placebo and 300mg remained stable at 12 and 15 months, while the 150mg group improved between baseline and 15 months.
“We see that subjects on nilotinib performed better overall on motor testing and had a better quality-of-life measurement during the study than the placebo group. These are important observations suggesting that nilotinib stabilized the disease—a potential disease modifying effect that we haven’t observed with any other agents,” says Georgetown neurology professor Fernando Pagan, MD, medical director of the GUMC Translational Neurotherapeutics Program and principal investigator on this study.
“These clinical findings need confirmation through larger studies with more diverse populations,” adds Pagan, who also directs the Movement Disorders Clinic at MedStar Georgetown University Hospital.
The investigators wish to thank all study participants and their families who participated in this trial over two years and hundreds of clinic visits.
In addition to Pagan and Moussa, authors include Michaeline L, Hebron, MS; Barbara Wilmarth, RN; Wangke Shi, MS; Sanjana Mulki, MS; Tarick Kurd-Misto; Sara Matar, MS; Xiaoguang Liu, MD, Ph.D., and Jaeil Ahn, Ph.D., all of GUMC;; Yasar Torres-Yaghi, MD; Abigail Lawler, MD; Elizabeth E Mundel, MD; Nadia Yusuf, MD; Nathan J Starr, MD; Muhammad Anjum, MD; of GUMC and MedStar Georgetown University Hospital; and Joy Arellano, RN; Helen H Howard, RN; of MedStar Georgetown University Hospital.
Georgetown holds an issued US patent for the use of nilotinib for the treatment of certain neurodegenerative diseases and has other pending patent applications in US and foreign jurisdictions. Moussa is the named inventor on the intellectual property.
Laboratory analysis from the first arm of the phase II clinical trial, published March 12, 2019 in the journal Pharmacology Research & Perspectives, showed that a single low dose of nilotinib reduces levels of a toxic protein that prevents the brain from utilizing dopamine that is stored in tiny vesicles, or pockets, in brain areas that may control movement.
Source: Read Full Article