Treatment guidelines for children hospitalized with COVID-19 were rapidly but not completely followed

Uptake of national guidelines for the treatment of children hospitalized with COVID-19 fell well below what would typically be expected, report researchers at the Medical University of South Carolina (MUSC) and elsewhere in Pediatrics.
The researchers looked at the medical records of children with COVID-19 at 42 children’s hospitals across the country before and after the release of national guidelines in 2020 to see how pediatricians’ prescribing habits changed. Although the use of recommended medications quickly increased, pediatricians still prescribed medications in accordance with the guidelines in only 55% to 82% of cases, depending on the type of medication and severity of the infection.
“This suggests our efforts with COVID-19 in children are not over,” said Ronald Teufel, M.D., director of Pediatric Hospital Medicine at the MUSC Shawn Jenkins Children’s Hospital and senior author of the study. Julianne Burns, M.D., a clinical assistant professor at Stanford University School of Medicine, is first author of the study.
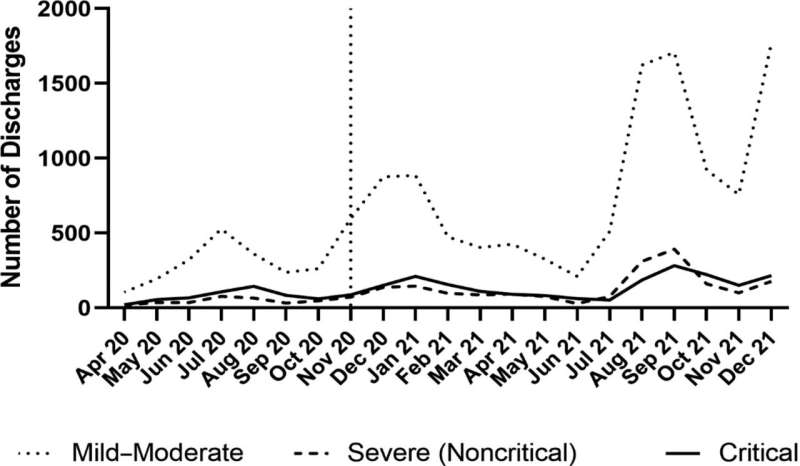
The study looked at the medical records of 18,364 children hospitalized with COVID-19, finding that 2,500 of those children had severe or critical disease. Severe disease typically means that children need oxygen delivered through a tube inserted at the tip of their noses. Critical disease often means that children need a breathing machine known as a ventilator. Although those children made up only a small percentage of COVID cases, the disease’s impact on them and their families was profound.
“While COVID is frequently thought of as a disease in adults, many of the children in this study required a stay in the intensive care unit, with very invasive medical care,” said Teufel. “This was not only terrible for each of the children, it also negatively impacted their parents, siblings, aunts, uncles, grandparents, friends and so many others.
In the early days of the pandemic, many medications were touted to prevent severe or critical disease, but little evidence was available to pediatricians about which were most effective. What evidence there was came from clinical trials in adults, leaving pediatricians with few options other than to apply these findings in children or rely on their own clinical experience and that of other physicians about what seemed to work.
In December 2020, the Infectious Diseases Society of America (IDSA) published evidence-based national treatment guidelines for children with COVID-19. Most children would require only supportive care, but the IDSA made specific recommendations for the care of children with severe or critical disease.
The IDSA guidelines endorsed the use of steroids, commonly used to decrease inflammation, in both severe and critical cases of COVID-19 but recommended the antiviral remdesivir only for the severe group. Few studies have tested remdesivir in critical cases, and results have been mixed, said Teufel. Existing evidence generally supports its efficacy early in the illness. However, it is less clear that it benefits patients with critical disease who are on a ventilator, he said.
These guidelines were followed much more quickly than is typical for guidelines for non-COVID-19 diseases. The tremendous impact of COVID-19 on the health, cultures and finances of people worldwide certainly provided enough motivation for clinicians to be educated on the most effective treatment options, Teufel said. When more reliable data came out, the pediatricians listened.
“Generally, people did the right thing,” said Teufel. “They stopped using things that were unproven and started using things that were more proven.”
For instance, they began using steroids and remdesivir more and ivermectin and the antimalarial hydroxychloroquine less.
However, the use of steroids topped out at 82%, which is interesting because these medications are readily available, and providers are very familiar with their use, Teufel explained.
The compliance with guideline recommendations for remdesivir was far lower. In about 59% of critical cases, pediatricians followed the guidelines and did not prescribe remdesivir. In about 55% of severe cases, they prescribed remdesivir, as the guidelines recommended. Adoption of all of these recommendations fell well short of the 90% or more typically expected for such guidelines.
Teufel would like to see those percentages tick up and reach a 90% adoption rate. However, he fears that percentages could instead drop as COVID is no longer in the news and top of everyone’s mind. He thinks that technology could be the answer. Building guideline-recommended order sets into the electronic health record across children’s hospitals would make it easier for pediatricians to prescribe the appropriate medications. Those order sets could be revised as guidelines evolve.
“COVID-19 will likely spike again over the next years,” said Teufel. “Let’s make sure we do the best we can to ensure our kids get great care.”
More information:
Julianne E. Burns et al, Medications and Adherence to Treatment Guidelines Among Children Hospitalized With Acute COVID-19, Pediatrics (2022). DOI: 10.1542/peds.2022-056606
Journal information:
Pediatrics
Source: Read Full Article