Researchers map rural U.S. counties most vulnerable to COVID-19

A county-by-county analysis of the United States by Princeton University researchers suggests that rural counties with high populations of people over 60 and limited access to health care facilities could eventually be among the hardest hit by the coronavirus pandemic (COVID-19) that has so far killed more than 100,000 people worldwide.
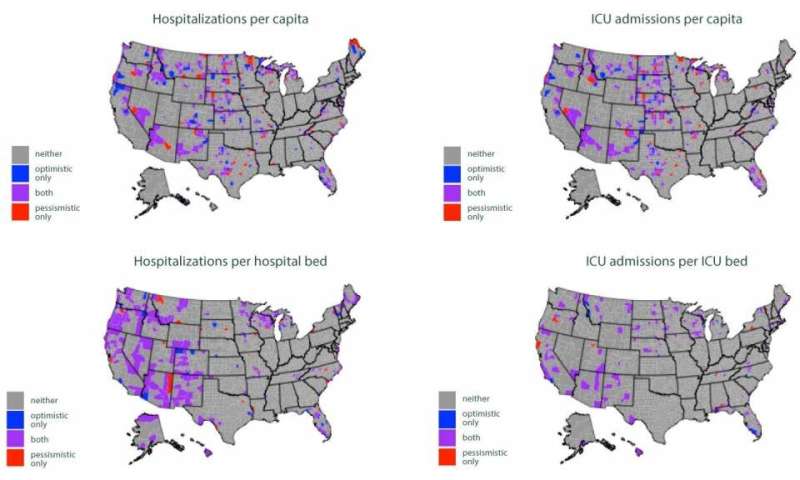
Counties concentrated in the western United States, the northern Midwest, Florida, and northern New England would have the highest ratios of hospitalizations to number of people, according to a paper published April 11 on medRxiv, a preprint database run by Cold Spring Harbor Laboratory, Yale University and BMJ. The researchers conclude that allocating emergency resources to hospitals and communities away from major population centers could be crucial to mitigating COVID-19.
“The burden is still going to be high in urban areas and the absolute number of cases will be highest in cities, but we could see rural areas have a higher per capita burden and a higher ratio of cases to hospital beds,” said first author Ian Miller, a graduate student in ecology and evolutionary biology at Princeton.
Miller and co-author Alexander Becker, also a graduate student in ecology and evolutionary biology, explained that hospitals—and particularly intensive care units (ICUs)—are unevenly distributed nationwide, with many regions having limited or even no facilities capable of providing the care needed to treat severe cases of COVID-19.
“We’re hoping that our study will prompt state and public health officials to keep an extremely close eye on rural areas,” said Miller, adding that he and his co-authors have been advising and consulting with officials in Missouri and shared their results with officials in Pennsylvania. “If they know where the vulnerable counties are, they can allocate resources to those counties, or try to help direct cases originating in those counties to health systems with more adequate capacity.”
Miller and Becker co-authored the paper with epidemiologists C. Jessica Metcalf, an assistant professor of ecology and evolutionary biology and public affairs, and Bryan Grenfell, the Kathryn Briger and Sarah Fenton Professor of Ecology and Evolutionary Biology and Public Affairs. Metcalf and Grenfell are associated faculty in the Princeton Environmental Institute (PEI) and affiliated with PEI’s Climate Change and Infectious Disease initiative, which has been focused on research related to coronavirus.
The researchers conducted an epidemiological simulation that compared how many hospital and ICU beds each county currently has—according to the American Hospital Association—to the number of coronavirus cases they would experience if the infection rate reaches 20% of the county’s population.
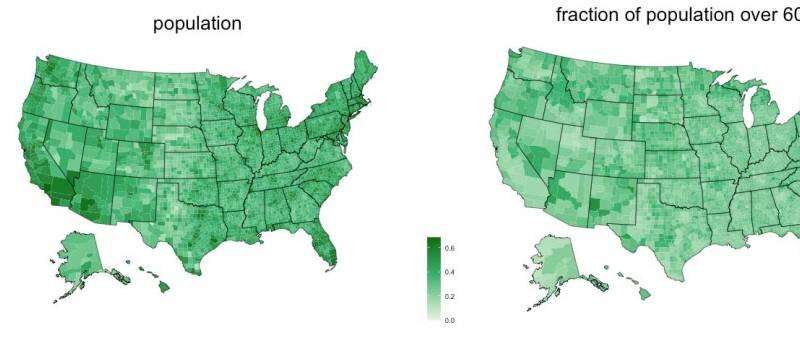
Using 2018 demographic data from the U.S. Census Bureau, the researchers broke down each county’s population by age group, starting at 0-9 and continuing every 10 years through the final designation of 70-plus. Their model then factored in the proportion of each age group that has been likely to become severely ill, with people over 60 being the most vulnerable.
The researchers ran two scenarios. In the “optimistic” scenario, disease transmission was relatively slow, people had contact mostly with those within their age group, and people presenting symptoms of coronavirus were effectively quarantined. In contrast, the “pessimistic” scenario was characterized by a high transmission rate, homogenous contact between different age groups, and people showing signs of infection being quarantined too late or not at all.
The counties that became overwhelmed in both the optimistic and the pessimistic scenarios are those that the study authors identified as most vulnerable to the current outbreak.
The Princeton study comes at a time when—after being largely concentrated in major coastal cities—coronavirus infections are starting to climb in rural areas. As of April 10, the virus had reached nearly three-quarters of the country’s rural counties, with the case rate being nearly double what it was six days earlier, according to the New York Times. Meanwhile, the last states to issue stay-at-home orders are among those with counties lacking in-county health care facilities.
“The idea that rural areas are immune to coronavirus is not the reality,” Becker said.
“Because people’s needs are so different within a state, that motivated us to look at the county level to get as high a resolution as we could,” he said. “Maybe these results can be used as a preparation guide for officials in counties that are at risk, especially if there’s a large distance between a rural area and an urban area with greater access to health care.”
“We’re not trying to tell public health officials to focus only on rural areas or only on urban areas,” Miller said. “We’re trying to give them a holistic picture of the burden all of the different parts of their state might face so they can try to provide equitable care.”
Source: Read Full Article