PSMA PET scanning can improve decision making for prostate cancer treatment
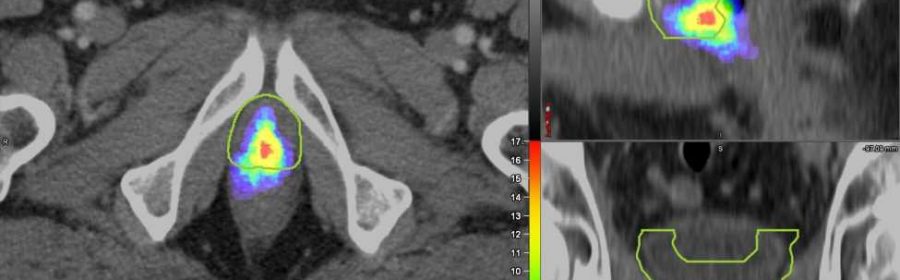
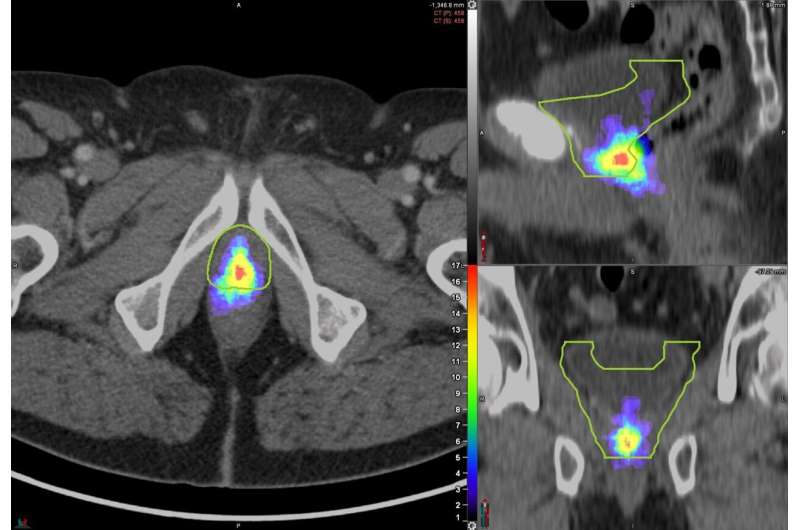
Detailed PSMA PET mapping of cancer recurrence in the prostate bed shows that current radiotherapy contouring guidelines—which determine the target areas for treatment—miss a significant number of lesions and may irradiate healthy tissues unnecessarily. In a new study published online by the Journal of Nuclear Medicine, researchers are calling for the redefinition of prostate bed contouring guidelines to improve outcomes for patients.
Approximately one-third of prostate cancer patients who undergo radical prostatectomy experience disease progression within 10 years. Salvage radiation therapy (SRT) is a potentially curative treatment option for these patients. SRT currently follows contouring guidelines based on expert consensus and does not take advantage of the information available from novel imaging techniques, such as PSMA PET.
“PSMA PET is one of the most accurate methods for detecting tumor recurrence after prostatectomy and, since its FDA approval in December 2020, has increasingly changed patterns of care for prostate cancer patients,” said Alan Dal Pra, MD, associate professor and director of clinical research in the Department of Radiation Oncology at the University of Miami Miller School of Medicine in Miami, Florida. “In our study, we sought to analyze the patterns of prostate bed recurrence with PSMA PET and see how they compared to current expert consensus contouring guidelines from the Radiation Therapy Oncology Group (RTOG).”
Researchers used PSMA PET to image the patterns of prostate bed recurrence in 127 prostate cancer patients experiencing PSA persistence or biochemical recurrence after radical prostatectomy. For each PSMA PET scan, researchers assessed the location of recurrent lesions and determined the clinical target volume (CTV) based on the RTOG contouring guidelines. The lesions were then categorized as completely covered, partially covered, or not covered by the contouring guidelines.
The recurrent lesions were completely covered in the CTV in 53% of patients, partially covered in 34% of patients, and not covered in 13% of patients. In addition, some areas in the CTV had no evidence of lesions at all.
“We hope this study will help redefine prostate bed contouring guidelines for SRT to improve the outcomes of patients receiving radiotherapy post-radical surgery,” stated Ida Sonni, MD, nuclear medicine physician and academic researcher in the Department of Radiological Sciences at the University of California, Los Angeles in Los Angeles, California. “Our work confirms the crucial and growing role that nuclear medicine and molecular imaging have in guiding decision-making for cancer treatment. Nuclear medicine plays an essential part in the multidisciplinary management of patients with prostate cancer and facilitates the use of individualized, tailored treatments, which ultimately benefit all our patients.”
More information:
Ida Sonni et al, PSMA PET/CT–based Atlas for Prostatic Bed Recurrence after Radical Prostatectomy: Clinical Implications for Salvage Radiation Therapy Contouring Guidelines, Journal of Nuclear Medicine (2023). DOI: 10.2967/jnumed.122.265025
Journal information:
Journal of Nuclear Medicine
Source: Read Full Article