What is CRIA syndrome?

Skip to:
- Symptoms & Pathology
- Causes and Current Research
- Treatment
Cleavage-resistant RIPK1-induced autoinflammatory (CRIA) syndrome, is a recently discovered autoinflammatory disease caused by mutations within the receptor-interacting serine/threonine-protein kinase 1 (RIPK1) gene.
The exact prevalence of CRIA syndrome is still undetermined as it has only recently been identified as a disease. Seven people from three separate families in the U.S. have been diagnosed with CRIA syndrome through genetic testing.
It is possible that many other people around the world could also potentially have CRIA syndrome.
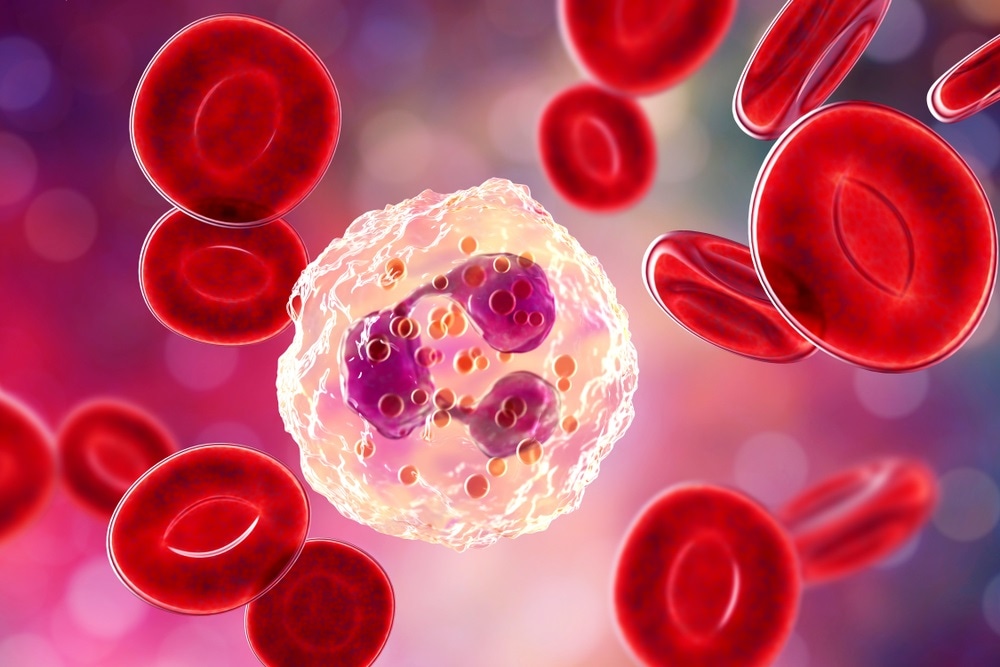 Image Credit: Kateryna Kon / Shutterstock.com
Image Credit: Kateryna Kon / Shutterstock.com
Symptoms & Pathology
The symptoms of CRIA syndrome are that of an autoinflammatory disease characterized by:
- Persistent episodic unexplained fevers – every 2-4 weeks from birth for 3-5 days
- Lymphadenopathy – painful swollen lymph nodes – related to the onset of fever
- Severe abdominal pains, gastrointestinal problems, and diarrhea
- Headaches
- Mouth ulcers & tonsillitis
- Enlarged liver and spleen (hepatomegaly & splenomegaly) – in some patients
None of the patients have rashes, genital ulcers, or arthritis, but some do have arthralgia (joint pain without swelling).
Causes and Current Research
Mutations in the RIPK1 gene cause CRIA syndrome. Typically, activation of RIPK1 controls inflammation pathways (innate immunity) mediated by a potent inflammatory mediator called tumor necrosis factor (TNF).
RIPK1 ensures that the inflammatory response to TNF is controlled and suitable to the level of inflammatory signaling by being altered post-transcriptionally.
Cleavage of RIPK1 at specific residues at D324 and D325 by caspase-8 separates RIPK1s kinase domain from its intracellular death domain; inactivating it, to potentially prevent necroptosis and apoptosis (though the mechanisms behind this is still unclear).
Specific autosomal-dominant heterozygous missense mutations change the residue at D324 to D324N, D324H & D324Y (the three mutations found in the three separate families) and D324V found in a separate study; all prevent caspase-8 cleavage of RIPK1 thus permanently activating RIPK1 leading to CRIA syndrome, also termed intermittent lymphadenopathy.
All of these missense mutations affecting D324 in RIPK1 are heterozygously inherited, meaning that there is still one fully functioning allele (normal gene variant). Still, among the affected individuals, the second allele is mutated second. When scientists engineered Ripk1D325A/D325A mice (meaning they have two mutated gene variants), these mice died embryonically during development. Mice with one mutated allele and one normal allele (Ripk1D325A/+), like human patients, survived and appeared healthy, although they were hypersensitive and hyperresponsive to inflammation.
Treatment
The typical course of treatment for people with autoinflammatory diseases are specific anti-inflammatory and immunosuppressive drugs, such as tocilizumab (an anti-IL6R antibody normally used to treat rheumatoid arthritis – another major autoinflammatory disease). While this may work for some CRIA syndrome patients in reducing systemic inflammation, specific RIPK1 inhibitors (currently under development) may be more suitable to treat this condition as its cause is monogenic potentially.
Sources:
- Lalaoui et al., 2020. Mutations that prevent caspase cleavage of RIPK1 cause autoinflammatory disease. Nature. 577(7788):103-108. https://www.ncbi.nlm.nih.gov/pubmed/31827281
- Tao et al, 2020. A dominant autoinflammatory disease caused by non-cleavable variants of RIPK1. Nature. 577(7788):109-114. https://www.ncbi.nlm.nih.gov/pubmed/31827280
- NIH.gov (2020). NIH researchers discover new autoinflammatory disease and uncover its biological cause. www.nih.gov/…/nih-researchers-discover-new-autoinflammatory-disease-uncover-its-biological-cause
Further Reading
- All CRIA Syndrome Content
Last Updated: Feb 17, 2020

Written by
Osman Shabir
Osman is a Neuroscience PhD Research Student at the University of Sheffield studying the impact of cardiovascular disease and Alzheimer's disease on neurovascular coupling using pre-clinical models and neuroimaging techniques.
Source: Read Full Article