Investigational drug may improve stem cell transplantation for multiple myeloma patients
The standard treatment for patients with multiple myeloma often includes stem cell transplantation in which the patient’s own stem cells are harvested and stored while the patient receives intensive chemotherapy to kill the cancer. Then, the patient’s stem cells are returned to the patient to help with recovery. But for a significant proportion of patients, the number of stem cells that can be harvested is not optimal for transplant and negatively affects patient outcomes.
However, an international phase 3 clinical trial led by physicians at Washington University School of Medicine in St. Louis has shown that the investigational drug motixafortide — when combined with the standard therapy for mobilizing stem cells — significantly increases the number of stem cells that can be harvested, compared with treatment with the standard agent alone. If approved by regulatory agencies, the combination with motixafortide potentially would improve the stem cell transplantation process for multiple myeloma patients.
Findings from the clinical trial are published April 17 in the journal Nature Medicine. The clinical trial was sponsored by the biopharmaceutical company BioLineRx Ltd., which makes motixafortide, and the National Institutes of Health (NIH).
“Stem cell transplantation is central to the treatment of multiple myeloma, but some patients don’t see as much benefit because standard therapies can’t harvest enough stem cells for the transplant to be effective,” said senior author John F. DiPersio, MD, PhD, the Virginia E. & Sam J. Golman Professor of Medicine. DiPersio treats patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine. “This study suggests motixafortide works extremely well in combination with the standard drug, granulocyte colony stimulating factor (G-CSF), in mobilizing stem cells in patients with multiple myeloma. The study also found that the combination worked rapidly and was generally well-tolerated by patients. We are hopeful that this investigational drug, if approved, will expand the number of patients who can receive an effective stem cell transplant for multiple myeloma.”
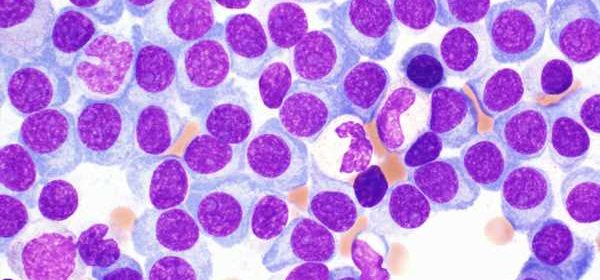
Multiple myeloma is a cancer of the blood and bone marrow. Some patients respond well to initial treatment, including chemotherapy and stem cell transplantation, but nearly all eventually relapse. On average, patients live four to seven years after diagnosis. A minimum of 2 million stem cells per kilogram body weight are necessary for a stem cell transplant in patients with multiple myeloma, but greater than 5 million to 6 million stem cells per kilogram body weight is considered optimal.
According to the researchers, including first author Zachary D. Crees, MD, an assistant professor of medicine and the assistant clinical director for the Washington University Center for Gene and Cellular Immunotherapy, the investigational drug motixafortide, when used in combination with the standard stem cell therapy, G-CSF, allowed optimal numbers of stem cells to be harvested in over 92% of patients after two collection procedures, compared with only 26% of patients who received G-CSF plus a placebo. Even after just one collection procedure, the data showed that optimal stem cell numbers could be collected from 88% of patients who received motixafortide plus G-CSF, compared with only 9% of patients who received standard G-CSF plus a placebo.
Compared with standard therapy alone, the researchers also found that stem cells harvested with motixafortide in combination with G-CSF showed a tenfold increase in the number of primitive stem cells that could be collected. Primitive stem cells have greater potential to develop into a wider variety of blood cell types, making them more effective at reconstituting red blood cells, white blood cells and platelets — all important for a patient’s recovery. Stem cells mobilized by motixafortide also showed increased expression of genes and genetic pathways associated with self-renewal and regeneration, all beneficial for increased effectiveness of a stem cell transplant.
In addition to their research in multiple myeloma, DiPersio and Crees also are evaluating motixafortide’s potential as a stem cell mobilizer to support the genetic correction of the inherited disease sickle cell anemia. This work is of particular importance because patients with sickle cell disease can’t be treated with G-CSF, the most common drug used for stem cell mobilization, due to dangerous side effects, including blocked blood vessels, organ failure and death. The hope is that development of a novel, effective and well-tolerated stem cell mobilizing regimen for a viral-based gene therapy approach using CRISPR-based gene editing will lead to improved outcomes for patients with sickle cell disease.
Even with initially effective stem cell transplants, multiple myeloma almost always recurs, and other types of therapies are in clinical trials to evaluate their effectiveness at managing this cancer. To further investigate therapies beyond stem cell transplants, the laboratories of DiPersio and Li Ding, PhD, the David English Smith Distinguished Professor of Medicine and a professor of genetics, along with the multiple myeloma program team led by Ravi Vij, MD, a professor of medicine, recently reported the first comprehensive genomic and protein-based analysis of bone marrow samples from multiple myeloma patients, specifically focused on finding potential targets for immunotherapies, such as chimeric antigen receptor T cells (CAR T), bispecific therapies and antibody drug conjugates (ADCs). The research identified new treatment targets that may expand the potential for immunotherapies to treat this cancer.
This work, led by multiple first authors including Lijun Yao, a doctoral student in Ding’s lab; Julia T. Wang, a doctoral student mentored by DiPersio and Ding; and Reyka G. Jayasinghe, PhD, an instructor in medicine, was published Feb. 13 in the journal Cancer Research. The study identified 53 genes that could prove promising in developing future therapies. Thirty-eight of these genes are responsible for creating abnormal proteins on the surface of multiple myeloma cells. These proteins could serve as targets for new immunotherapies; 11 of the 38 genes had not been identified previously as possible targets.
Source: Read Full Article