plastic coating in pills
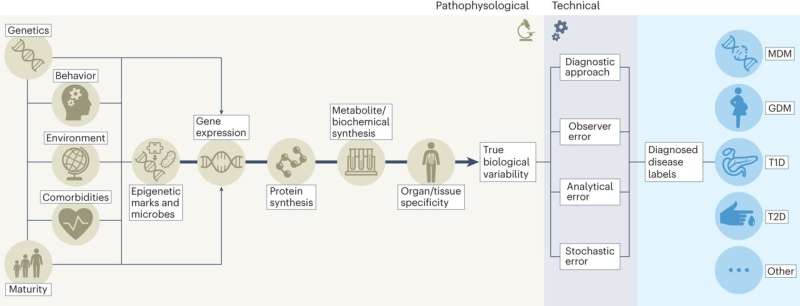
Diabetes can show up in almost anyone: pregnant women, babies, kids, teens, adults both young and old. But the condition’s various forms, liquid heart worm medicine all of which affect how the body processes blood sugar, can manifest quite differently in the hundreds of millions of people worldwide who have the disease—making it perfect for the individualized approach known as precision medicine, Stanford Medicine researchers say.
“Traditional medicine takes a one-size-fits-all approach to treatment and diagnostics,” said Jessie Wong, Ph.D., a clinical psychologist with the pediatric endocrinology team at Stanford Medicine Children’s Health. “That works well for some people but not others.” In contrast, precision medicine enables doctors to merge information on the patient’s type of diabetes with knowledge about their lives, charting an individualized course of treatment.
As part of a team of 200 academics from 28 countries, Wong helped write a comprehensive report on the state of precision medicine for diabetes.
The report, published in Nature Medicine, and accompanied by additional papers in Communications Medicine and The Lancet Diabetes & Endocrinology, summarized everything known about this personalized approach.
Three other Stanford Medicine diabetes experts—Anna Gloyn, DPhil, Korey Hood, Ph.D., and Jennifer Ikle, MD, Ph.D.—were also members of the team.
Wong spoke about the report’s key take-aways for precision medicine and type 1 diabetes treatment, the section of the report she helped produce.
Of the type 1 diabetes treatments you reviewed, which findings stood out?
We focused on diabetes technologies because they are at the forefront of what is considered standard for Type 1 diabetes management. Some of these technologies electronically link a patient’s continuous glucose monitor, including a glucose sensor inserted in the skin, to their insulin pump. The technology continuously monitors blood sugar and automatically administers and adjusts insulin doses.
It was great to see consistent benefit from these technologies for blood-sugar control, such as measurements of hemoglobin A1c, which can help assess the patient’s last three months of blood sugar levels, and “time in range,” the percent of time each day that blood glucose is in the target range.
The other component we found—something I think has been really understated—is the positive impact of the technology on people’s lives, including sleep quality and psychosocial well-being. We might think of these as auxiliary, but the truth is that when you are living with Type 1 diabetes, managing the disease impacts your entire life experience.
What does the quality-of-life finding mean for kids with type 1 diabetes and their families?
In the data on children, we found that continuous glucose monitoring devices can vary somewhat in their glycemic, or blood-sugar, benefits, with the most prominent benefit for older populations. But even though there was less glycemic benefit for younger children, there are a bunch of psychosocial benefits in that group—not only for the patients, but also for their parents.
Before the continuous monitoring devices were available, a parent might wake up a few times every night to check their child’s blood sugar, for years on end. With the devices taking over that task, parents sleep better, have less distress related to diabetes management and feel better emotionally, which not only benefits them but also makes them better caregivers for their children.
What are the gaps in our knowledge, and what should precision medicine studies focus on next?
There weren’t any studies that directly compared the same type of diabetes device or technology among brands. That’s not a coincidence; the studies are run by device manufacturers that have their own interests. But that type of research is necessary. Without head-to-head comparisons, it is harder to say to an individual patient, “This device is better for you based on these factors in your life.”
Few studies assessed whether there are subgroups of patients who have a more difficult time accessing diabetes technology, or the extent to which medical teams provide “tech support” for device use. These factors can greatly impact someone’s success at initiating the technology or continuing to use it.
We also saw a need for more research to understand how the technologies function—or don’t—for patients of different socioeconomic levels and from all racial and ethnic groups. Many of the existing study samples consist of non-Hispanic white patients with higher socioeconomic status.
The whole idea behind precision medicine is that considering these factors should improve equity in diabetes care and in medicine in general. But we need more studies that follow large, diverse samples of patients so we can find the relationships between their individual characteristics and their outcomes.
If a child with diabetes or a parent asked you what the report means for their family, what would you tell them?
We always say that diabetes care is an art and not a science because no one is going to experience diabetes exactly the way your child does, or you do. That’s really frustrating for people living with diabetes and their parents to hear; they want it to be a perfect equation where you plug in the numbers and you get out the exact answer that makes sense.
But precision medicine moves diabetes treatment closer to that ideal. We’re putting more variables into the equation about who you are, the life you live, your genetic background—all the factors that go into the way that diabetes is part of your life. Those factors add valuable information so we can ensure we’re treating your diabetes the best way possible. The best approach is not going to be the same for everybody; we want to get to what’s best for you.
Are there other specialties where you have seen precision medicine applied and thought, ‘I wish we were doing that in diabetes care?’
It’s so funny you say that, because I always feel that way in reverse! I’ve had colleagues in other subspecialties say that they’ve used diabetes as their model for putting precision medicine into action.
Whether it’s integrated multidisciplinary care within the clinics, or including psychosocial interventions along with medical education, or the technology we can offer our patients, diabetes has consistently been at the forefront of using precision medicine to help the people we take care of.
More information:
Deirdre K. Tobias et al, Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine, Nature Medicine (2023). DOI: 10.1038/s41591-023-02502-5
Journal information:
The Lancet Diabetes & Endocrinology
,
Communications Medicine
,
Nature Medicine
Source: Read Full Article