legal nolvadex substitute
How revolutionary rethink in the way prostate cancer is diagnosed may reassure men it is safe to postpone having treatment – as experts call for early stage disease to be reclassified as pre-cancer
- Experts have said earliest stage prostate cancer to be called ‘pre-cancer’
- 50,000 men told they have disease a year in the UK, but this could half it
A radical rethink in the way prostate cancer is diagnosed could be on the cards – with experts calling to reclassify the earliest stage tumours as ‘pre-cancer’, The Mail on Sunday has learned.
Every year roughly 50,000 men in the UK are told they have the disease, buy online viagra super force au pharmacy and the move would effectively see this figure cut in half.
Mounting evidence suggests patients with these tiny tumours don’t usually need to start treatment. Instead they can simply be monitored with regular blood tests and scans to ensure the tumours don’t start to spread.
This approach is now offered to about 90 per cent of men when newly diagnosed with prostate cancer, with the aim of sparing them from complications following invasive surgery and radiotherapy, which can include incontinence and erectile dysfunction.
A major study published last month proved that survival rates for the group who are monitored are the same as for those given more aggressive traditional treatment.

A radical rethink in the way prostate cancer is diagnosed could be on the cards – with experts calling to reclassify the earliest stage tumours as ‘pre-cancer’
While experts admit that it feels ‘counterintuitive’ to not treat a cancer, many small, early-stage prostate tumours are so slow-growing that it could be many years before they begin to spread. And some never do. And if doctors spot signs that the disease is on the march, more definitive treatment could be quickly given.
Despite this, not all men are convinced. Cancer specialists say around one in ten push for invasive therapies as soon as they’re diagnosed, even when told they don’t need them.
The hope is that the reclassification of early-stage tumours as pre-cancer would help to reassure this group that waiting is a better option and will give them more healthy years – free from the sometimes life-changing problems that often occur after treatment.
‘The majority of men recommended monitoring have low-level prostate cancer which is in no danger of ever leaving the prostate and becoming life-threatening,’ says Joe O’Sullivan, professor of radiation oncology at Queen’s University Belfast and an authority on the treatment of prostate cancer.
‘If you actively looked for this form of cancer in the population you’d find it in most men over the age of 60. But if you tell a patient they have cancer, that’s always going to make them nervous.’
He adds: ‘Of course, these early-stage prostate cancers are still – scientifically speaking – cancer, but in a practical sense they are not. The tumour is not invasive and it is highly unlikely to spread.
‘It would be game-changing for my patients if I could tell them that all they have is a form of pre-cancer. This is why there is this growing conversation about reclassifying some forms of the disease.’
The Mail on Sunday has discovered this is indeed an issue that is being widely debated.
Last week, in her column, our resident GP Dr Ellie Cannon reassured a reader who’d written in expressing his fears about ‘going untreated’. She told him that it was safe to watch and wait – but scores of men either wrote to us or commented online after reading the article to say they too weren’t happy being told they had to live with cancer.
One recently diagnosed prostate cancer patient, Steven Griffiths, 72, said that putting off treatment until later in life worried him because he fears he will not cope as well with surgery or radiotherapy in his 80s. He is deciding whether to undergo surgery to remove his prostate this year rather than wait.
Meanwhile, 85-year-old Peter Giles said he wishes he’d had surgery to remove his prostate cancer when it began to spread when he was in his 60s. He waited instead, which meant he had to undergo intensive treatment and was left with lifelong problems.
And given that 11,000 British men die from prostate cancer each year, aren’t the concerns justified?
Experts – who insist that prostate cancer is one of the best-understood diseases treated on the NHS – say not.
IT’S A FACT
For every 10cm put on around the waist, the likelihood of a man developing high-grade prostate cancer increases by about 13 per cent.
Usually it is picked up with a prostate specific antigen (PSA) blood test – which checks for high levels of a protein that indicates that the prostate is not functioning as it should – and an examination.
As the disease is more common in men over 50, GPs might suggest these tests on an ad hoc basis, or they may recommend the test if the patient is suffering any symptoms of prostate problems, such as changes to patterns in urination.
If prostate cancer is suspected, scans and a biopsy – where a sample of tissue from the prostate is removed and examined under a microscope – can confirm the diagnosis. These are used to determine the stage – how large the tumour is and how far it has spread – and the grade – how rapidly it’s growing.
Prostate cancer is graded using a system known as the Gleason score. A score of one is considered normal. Between two and five is ‘at risk’ but not cancer. A six or a seven means the tumour is slow growing and a score of eight to ten – the limit of the scale – would be deemed fast-growing.
This score, along with scan and blood test results, are used to decide whether the prostate cancer is low, medium or high risk.
High-risk patients are recommended treatment – such as surgery or radiotherapy – while the NHS watchdog the National Institute for Health and Care Excellence says low- and medium-risk men are also offered the option of monitoring only.
The reason doctors believe it’s a safe bet is largely thanks to a major, ongoing trial that has been tracking 1,600 patients with low- and medium-risk prostate cancer.
The latest data from the trial, published last month, found these men have just as good a chance of surviving for 15 years regardless of whether they opted for monitoring, surgery or radiotherapy.
‘This trial was a big deal,’ says Dr Alison Tree, consultant clinical oncologist at The Royal Marsden. ‘We know a lot about prostate cancer now and how it behaves. This means we’ve been able to improve survival rates and also be confident about resisting treating patients unnecessarily.’
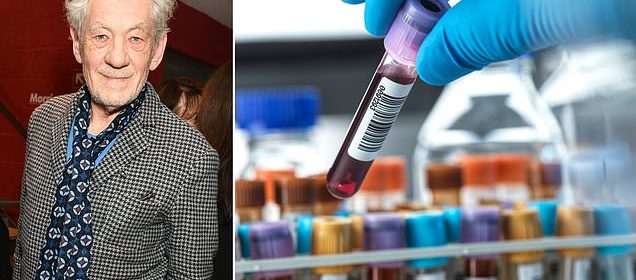
Monitoring involves regular scans and PSA tests to keep tabs on whether the tumour is growing. Sir Ian McKellen, 83, is a case in point. The veteran British actor, who played the wizard Gandalf in The Lord Of The Rings movies, was diagnosed with slow-growing prostate cancer in 2006. He has avoided aggressive therapies, opting instead for frequent checks to make certain the cancer has not got worse.
If any worrying changes are spotted, patients will typically be recommended radiotherapy or surgery. In the study, around three-quarters of men who started out being monitored went on to have these treatments.
Experts say this shows that any changes which occur during surveillance are promptly picked up and dealt with.

CHECK UPS: Sir Ian McKellen has his prostate tumours monitored
If a patient has underlying health problems that would make aggressive treatment more risky – such as high blood pressure – or someone is considered close to the end of their life, doctors may suggest hormone therapy.
This involves taking drugs with the aim of slowing the progression of the disease, rather than curing it. If this doesn’t work, radiotherapy or surgery is still an option.
‘There is no age cut-off,’ says Prof O’Sullivan. ‘Men in their 90s can get surgery or radiotherapy if doctors judge it is necessary and safe,’ he says.
Despite this, Dr Ben Lamb, consultant prostate surgeon at Bart’s Health NHS Trust, says: ‘Some men can’t handle the idea of living with cancer and it’s up to them to decide the best course of action. While we do our best to explain that they are better off on active surveillance, we give intensive treatment to roughly ten per cent of these patients because it’s their preference.’
IT’S A FACT
Over the past decade, prostate cancer incidence rates in the UK have increased by roughly eight per cent.
Experts also say doctors, nervous about missing their chance to catch the cancer, may recommend treatment unnecessarily.
‘It’s not just patients who can push for unnecessary treatment, – clinicians can also go too early with invasive procedures too,’ says Prof O’Sullivan.
Reclassifying the lowest risk prostate cancers – with a Gleason score of six – as pre-cancer could help reduce this anxiety. Research suggests about 98 per cent of these tumours – known as Gleason six tumours – do not grow or spread outside the prostate so should no longer be considered cancer.
‘This is the least aggressive form of prostate cancer that is incapable of causing symptoms or spreading,’ said Dr Scott Eggener, urologist at the University of Chicago and lead author of a study calling for Gleason six tumours to be reclassified as pre-cancer.
The charity Prostate Cancer UK says it is supportive of the idea.
‘Prostate cancer can be a huge diagnosis and many men worry about the safety of being on active surveillance,’ says Emma Craske, senior specialist nurse at Prostate Cancer UK. ‘This psychological weight can drive men to seek treatment even if they don’t need it.
‘Given how unlikely a Gleason six tumour is to spread, it could be a good idea to recategorise them.’
Patients themselves are split over the decision. In February, a Canadian survey of 450 prostate cancer patients found that 35 per cent supported reclassifying Gleason six as ‘low-risk prostate lesions’ but 35 per cent opposed it, with the rest undecided. Opponents of the change argue it might lead to men dropping out of monitoring altogether. But the survey found eight in ten men said they would continue with surveillance, even if told they had pre-cancer rather than cancer.
Despite this, Dr Lamb is unconvinced. ‘Gleason six tumours are cancerous and it would be dishonest to say they’re not,’ he says.
‘The NHS needs to improve counselling prostate cancer patients after diagnosis, by properly explaining their options with facts and figures. That is better than fudging the definition of cancer.’
And what of all those worrying prostate cancer deaths?
In most of these cases, the tumour was picked up late, once the cancer had already spread to nearby organs such as the bladder and pelvis. One in ten prostate cancers are discovered at this stage – when the disease is incurable – because patients seek help too late. A small proportion of men suffer aggressive cancers that, even when detected early, spread fast and are quickly fatal. Around half of men with advanced prostate cancer survive five years.
Experts say this is an area where research progress still needs to be made.
‘Every year we see patients whose prostate sadly isn’t going to be treatable, even with early surgery and radiotherapy,’ says Dr Lamb.
‘We need to get better at working out who is most at risk of these cancers, for example if they have genes which make aggressive cancer more likely.’
Some of those with low-risk cancer who push for treatment may come to regret it.
One of them is Harry Norman, 74, from Manchester, who underwent surgery to remove his prostate in 2019 and found it left him with debilitating side effects.
He was diagnosed in 2018 after his GP advised him to take a PSA test. He had no symptoms and his consultant advised active surveillance – but Harry chose surgery.
‘He thought it would be best to get it out of the way,’ says his wife Jane, 74. ‘He didn’t want to live with the anxiety of having cancer and I supported the decision. Looking back, we bitterly regret it.’
While the surgery removed the cancer, there was an uncommon complication which left him with permanent bowel problems.
‘His bladder often gets blocked so he can’t pee,’ says Jane. ‘He’s now got a permanent catheter and he regularly needs to go to hospital to have this adjusted. We can’t go on holiday and he struggles to leave the house.
‘People aren’t aware of the risks of this surgery. If it’s a life-saver, it’s worth it, of course. But it’s not a one-time thing which removes all your worries. There are lots of things that can go wrong.’
Source: Read Full Article