doxycycline canine injection side effects
As effective as catheter ablation can be for patients with paroxysmal atrial fibrillation (AF), the procedure that aims for pulmonary vein isolation (PVI) has met much less success in those with persistent AF, when episodes last a week to a year or more.
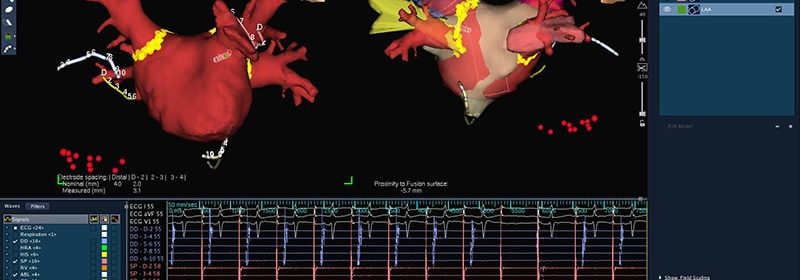
To boost catheter ablation’s chances for success in persistent AF, PVI is often augmented with further ablation to achieve posterior wall isolation (PWI). But the add-on strategy has had mixed success in the literature, how to take valacyclovir 1 gram and a newly published randomized trial has done little to improve its record.
The addition of PWI to PVI emerged as no better than solo PVI at suppressing atrial arrhythmias over 1 year in the international CAPLA trial, arguing against its routine use in patients like the trial entered: symptomatic with drug-refractory persistent AF undergoing their first AF ablation procedure.
Posterior wall isolation “I suspect is themost common add on-strategy to pulmonary vein isolation in patients with persistent atrial fibrillation,” Peter M. Kistler, MD, the Alfred Hospital and Baker Heart and Diabetes Institute, Melbourne, Australia, told theheart.org | Medscape Cardiology. “I’ve been doing it for more than 10 years,” he said, based on supportive observational studies.
But given the results of CAPLA, “I would express caution about empirically isolating the posterior wall in patients with persistent AF as a first-time ablation strategy,” said Kistler, who is lead author on the study’s January 10 publication in the Journal of the American Medical Association. He also presented the results in preliminary form last August at the European Society of Cardiology (ESC) Congress 2022.
Based on current evidence, he said, patients undergoing first-time ablation for persistent AF should receive PVI alone. In a potential exception, however, PVI plus ablation guided by markers for slow conduction may be more effective.
In the recently published, randomized ERASE-AF trial, for example, PVI plus individualized ablation guided by detection of atrial low-voltage myocardium suppressed atrial arrhythmias in patients similar to those in CAPLA.
And, possibly, PVI plus PWI may be more effective in selected patients with persistent AF, such as those with the arrhythmia for longer than 12 months. The few such patients in CAPLA, Kistler said, showed a nonsignificant trend favoring addition of PWI but, “One always wants to be careful in coming to conclusions based on subgroup analysis.”
“While disappointing,” states an accompanying editorial, “the failure of the CAPLA trial to demonstrate a significant improvement in outcomes is an important finding that should call into question the current understanding of the pathophysiology of persistent AF and the limitations of current techniques.”
Many patients with persistent AF do not show left atrial structural or electrographic evidence of “slow and heterogeneous” conduction, observes Rod Passman, MD, Northwestern University Center for Arrhythmia Research and Feinberg School of Medicine, Chicago.
“The benefit, therefore, of empirically isolating a seemingly healthy posterior wall in all patients with persistent AF may be limited,” he writes.
CAPLA randomly assigned 338 symptomatic adults (77% male) undergoing a first-time ablation for persistent AF at 11 centers in Australia, Canada, and the United Kingdom to PVI-only procedures or to ablation for PVI and PWI. Antiarrhythmic meds were allowed for 3 months after the procedure but were “discouraged” thereafter.
Unsurprisingly, mean procedural time was significantly shorter, by 21 minutes, among the 168 PVI-only patients compared to the 170 getting PVI plus PWI, as was the mean ablation time, by 6 minutes. Mean fluoroscopy times were similar, however.
Successful PVI was achieved in all patients, and 86% of the PVI plus PWI group had successful PWI. “There was zero procedural mortality, with no cerebrovascular events or esophageal fistula,” the report states.
The primary endpoint, “freedom from any documented atrial arrhythmia of more than 30 seconds without antiarrhythmic medication at 12 months after a single ablation procedure,” was met by 53.6% of solo PVI patients and 52.4% of the PVI plus PWI group (P = .98) at 1 year. Nor was there a significant difference in AF burden.
“For patients with symptomatic persistent AF, the CAPLA trial provides yet another disappointing result in the search for effective catheter-based therapies,” Passman writes.
“Whether new energy sources such as pulsed-field ablation or ultra–low temperature cryotherapy will provide durable transmural lesions that translate to better outcomes for this population remains to be seen,” he continues, “but their favorable risk profiles have provided needed optimism.”
Cryoablation is unlikely to improve PWI results, Kistler said, “because it’s very difficult to get good contact on the posterior wall with the balloon.”
But pulsed-field ablation catheters are often used for PWI, “and it seems like it’s quite effective.” That may be because they don’t pose a risk for thermal injury, such as to the esophagus, he observed, and therefore permit more thorough ablations.
Kistler reports receiving speaker fees from Abbott Medical and serving on an advisory board for Biosense Webster. Disclosures for the other authors are in the report. Passman reports receiving personal fees from Medtronic and Abbott Laboratories for serving on steering committees; receiving grants from Abbott Laboratories, the National Institutes of Health, and the American Heart Association for research on atrial fibrillation; and receiving royalties from UpToDate.
JAMA. Published online January 10, 2023. Full text, Editorial
Follow Steve Stiles on Twitter: @SteveStiles2. For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook.
Source: Read Full Article