Working conditions and non-workplace factors affect COVID-19 mortality in England

The COVID-19 pandemic has been severe in the United Kingdom, where infection and death rates were very high during both waves of the pandemic. While most deaths are among the elderly, many deaths have been reported among the working population, especially the essential workers. There have been many reports that suggested key occupational differences in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and death risk, but there have not been many systematic comparisons of death rates across different occupations.
SARS-CoV-2 infections among health care workers have drawn a lot of attention, and evidence shows that ICU workers caring for COVID-19 patients are at elevated risk of contracting the virus. However, other occupations such as those involving social care or public service may also be at increased risk of infection. Studies show that age-standardized mortality rates (ASMRs) for COVID-19 are high among bus and coach drivers, taxi drivers, sales and retail assistants, chefs, and social care workers.
Estimating occupational variations in COVID-19 mortality in England and Wales
Researchers from England recently estimated occupational variations in COVID-19 mortality in England and Wales during 2020 and examined how these differences changed post adjustment for non-workplace factors. The study's objective was to determine occupational differences in COVID-19-related mortality and assess if these differences are confounded by other factors, including ethnicity, regional differences, and education or non-occupation-related factors such as pre-pandemic health or deprivation. This study is published on the medRxiv* preprint server.
A total of 14,295,900 individuals living in private households in England in 2019 were part of the retrospective cohort study. The age of the participants ranged from 40 to 64 years, with a mean age of 52 years. 51% of the study participants were female, and all participants were employed in 2011 and completed the 2011 census.
The primary outcome measures were COVID-19 related mortality between 24 January 2020 and 28 December 2020. The researchers estimated ASMR per 100,000 person-years at risk stratified by occupations and sex. To determine the effect of occupation due to work-related exposures, they used Cox proportional hazard models to adjust for confounding factors such as ethnicity, region, and education, and non-workplace factors related to occupation.
Results show wide variations in COVID-19 mortality across occupations
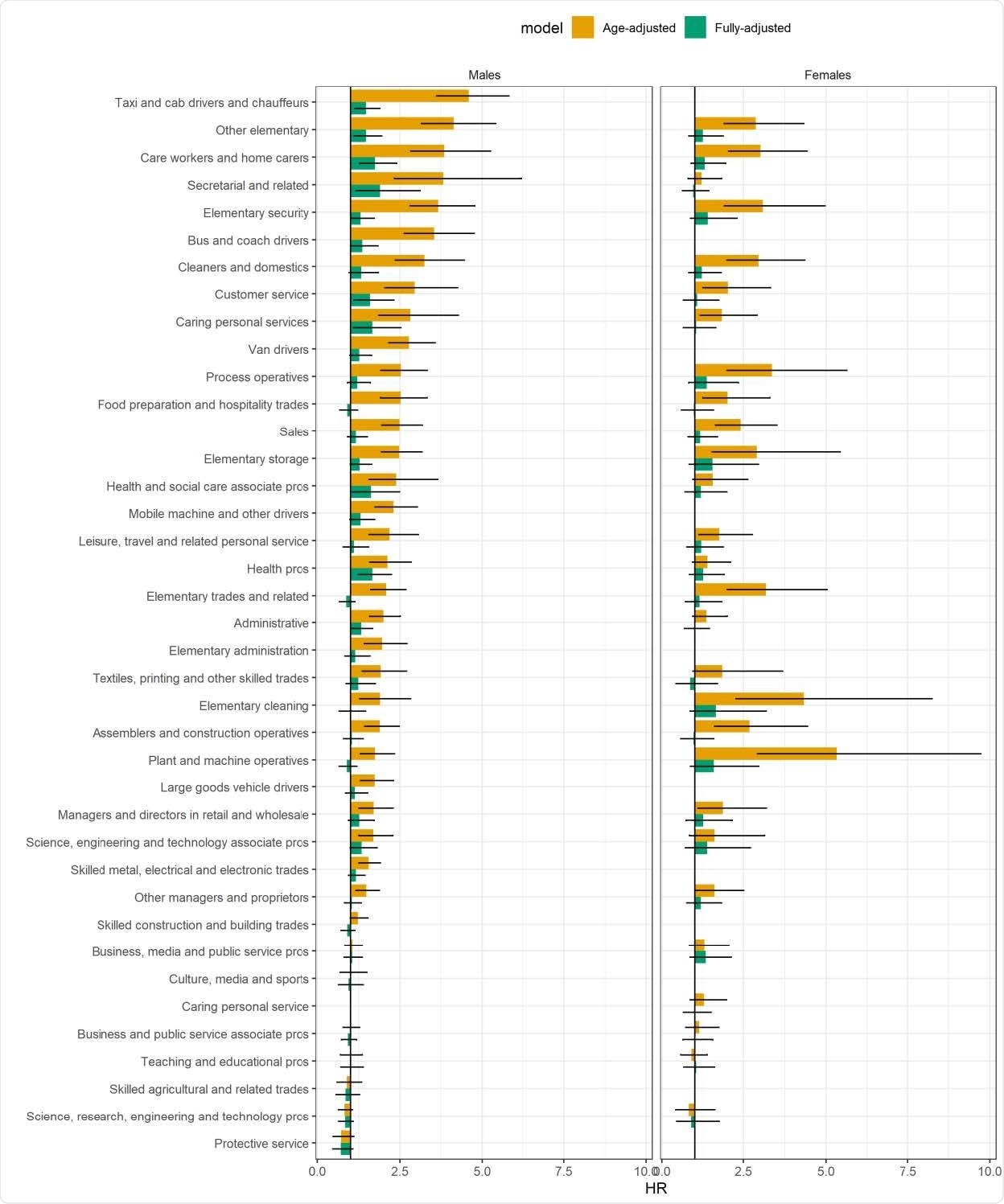
The results of the study show that there are vast differences in COVID-19 mortality across occupations. Many occupations, especially those involving contact with COVID-19 patients or the public, were shown to be at 3 or 4-fold more risk than other occupations.
"Our age-standardized mortality rates and age-adjusted hazard ratios confirm that there is a wide variation in the risk of COVID-19 mortality between occupations."
These elevated risks were significantly reduced after adjusting for mediating and confounding non-workplace factors. For instance, the hazard ratio for male taxi drivers or chauffeurs changed from 4.60 to 1.47 after adjustment. On comparing men in essential and non-essential occupations, the overall hazard ratio decreased from 1.45 to 1.22 after adjustment. For most occupations, confounding and mediating factors explained nearly 70% to 80% of the age-adjusted hazard ratios.
"Our analyses have confirmed previous findings that many occupations have elevated risks of COVID-19 mortality."
Non-workplace factors such as socio-demographics, region, and pre-pandemic health also affect COVID-19 mortality
The study's findings show that occupation and working conditions are likely to affect COVID-19 mortality, more so in occupations that involve contact with the public or COVID-19 patients. However, there is also a significant contribution from non-workplace factors such as socio-demographic factors, region, and pre-pandemic health status.
"A number of occupations showed increased risks, even after comprehensive adjustment, and working conditions likely played a role. However, our findings also indicate that non-workplace factors also play a major role."
Thus, preventive measures are urgently needed to minimize workplace exposures to SARS-CoV-2, and also to reduce exposure to the virus due to other factors such as inadequate housing, overcrowding, and deprivation.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Occupation and COVID-19 mortality in England: a national linked data study of 14.3 million adults Vahé Nafilyan, Piotr Pawelek, Dan Ayoubkhani, Sarah Rhodes, Lucy Pembrey, Melissa Matz, Michel P Coleman, Claudia Allemani, Ben Windsor-Shellard, Martie van Tongeren, Neil Pearce medRxiv 2021.05.12.21257123; doi: https://doi.org/10.1101/2021.05.12.21257123, https://www.medrxiv.org/content/10.1101/2021.05.12.21257123v1
Posted in: Men's Health News | Medical Research News | Women's Health News | Disease/Infection News
Tags: Coronavirus, Coronavirus Disease COVID-19, Education, Health Care, Mortality, Pandemic, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Social Care, Syndrome, Virus

Written by
Susha Cheriyedath
Susha has a Bachelor of Science (B.Sc.) degree in Chemistry and Master of Science (M.Sc) degree in Biochemistry from the University of Calicut, India. She always had a keen interest in medical and health science. As part of her masters degree, she specialized in Biochemistry, with an emphasis on Microbiology, Physiology, Biotechnology, and Nutrition. In her spare time, she loves to cook up a storm in the kitchen with her super-messy baking experiments.
Source: Read Full Article