Vaccine apartheid caused by gap in access between richer and poorer countries
While the worst of the COVID-19 pandemic is behind us, research continues on the role of vaccines—their effectiveness as well as factors that contribute to a resistance to being vaccinated, and the worldwide availability of the vaccine.
A new study co-authored by Ashely Fox and published this month in Health Affairs looks at “vaccine apartheid”—the gap in access to COVID-19 vaccines between high- and low-income countries.
Fox, an associate professor in the Department of Public Administration & Policy at UAlbany’s Rockefeller College, was lead author of the study, “Substantial Disparities in COVID-19 Vaccine Uptake and Unmet Immunization Demand in Low- and Middle-Income Countries,” co-written by Yongjin Choi and Leesa Lin, both of the Vaccine Confidence Project at the London School of Hygiene and Tropical Medicine.
The new study is among the first to quantify unmet demand for the vaccine—people who would be willing to be vaccinated if they had access. “By shedding light on the extent to which low uptake is due to constrained supply versus low demand, this study contributes to informed decision making and the development of targeted strategies to improve vaccine access and acceptance in low- and middle-income countries,” the article says.
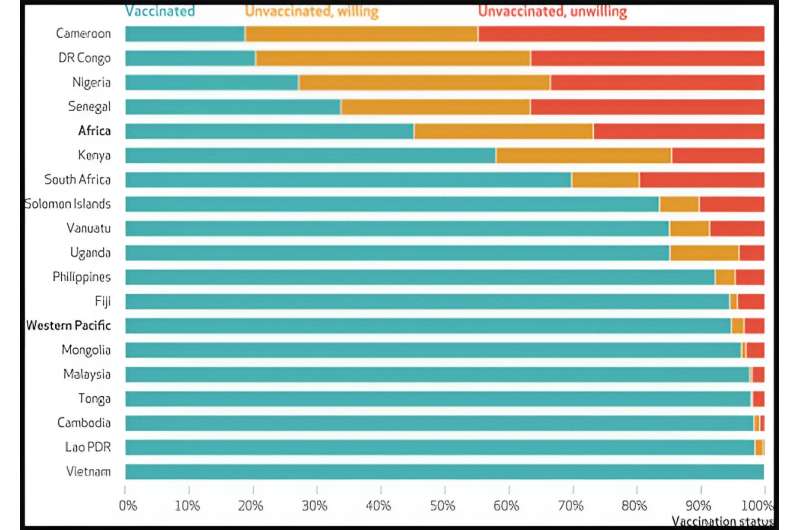
The study is based on surveys conducted between May 2022 and January 2023, at least a year after widespread vaccine roll-out, that collected data from 15,696 respondents in 17 Western Pacific and African countries. Results indicate that only about 50% of individuals in the Africa region had received primary vaccination and only 20% had received a booster shot. Only 22% of the entire sample had received an mRNA vaccine. Strikingly, the study found that among unvaccinated respondents, 50% were willing to be vaccinated but the shots were unavailable to them.
The surveys were conducted in Cambodia, Fiji, Lao People’s Democratic Republic Malaysia, Mongolia, the Philippines, Solomon Islands, Tonga, Vanuatu and Vietnam in the Western Pacific, and the African nations of Cameroon, the Democratic Republic of the Congo, Kenya, Nigeria, Senegal, South Africa and Uganda with support from the Vaccine Confidence Project. Unmet vaccine demand was highest in African countries, the study found, and lowest among the Western Pacific region.
The highest level of unmet demand was in the Democratic Republic of the Congo, at 43%, followed by Nigeria at 39% and Cameroon at 36%. Uganda and South Africa showed unmet demand of 11% in the population. In the Western Pacific countries surveyed, unmet demand was lower than 7%.
This correlates with the fact that as of May 2023, African countries had the lowest COVID-19 vaccine uptake, at 60 doses per 100,000 people. In contrast, Australia’s rate was 250 doses per 100,000—similar to South America and the European Union.
“Vaccine hesitancy and availability are much more interconnected than people often realize,” Fox said. “Low-income countries, especially in Africa, continue to experience constrained access to vaccines, including the more efficacious mRNA vaccines. People also have concerns about available vaccines. We need more research to understand both the supply and demand side factors that affect people’s willingness to vaccinate against COVID-19, and their continued willingness to vaccinate again.”
The article concludes that countries need targeted efforts to increase vaccination rates.
“Policy efforts should address barriers to vaccine access, ensure accessibility and distribution of mRNA vaccines, and aim to overcome vaccine hesitancy—all critical factors in reducing unmet immunization demand and achieving higher vaccination rates across regions.”
More information:
Ashley M. Fox et al, Substantial Disparities In COVID-19 Vaccine Uptake And Unmet Immunization Demand In Low- And Middle-Income Countries, Health Affairs (2023). DOI: 10.1377/hlthaff.2023.00729
Journal information:
Health Affairs
Source: Read Full Article