Study of NCOA3 yields novel findings of melanoma progression

For the first time, activation of nuclear receptor coactivator 3 (NCOA3) has been shown to promote the development of melanoma through regulation of ultraviolet radiation (UVR) sensitivity, cell cycle progression and circumvention of the DNA damage response. Results of a pre-clinical study led by Mohammed Kashani-Sabet, M.D., Medical Director of the Cancer Center at Sutter’s California Pacific Medical Center (CPMC) in San Francisco, CA were published online today in Cancer Research, a journal of the American Association for Cancer Research.
“Our research suggests a previously unreported mechanism by which NCOA3 regulates the DNA damage response and acts as a potential therapeutic target in melanoma, whereby activation of NCOA3 contributes to melanoma development following exposure to ultraviolet light,” says Dr. Kashani-Sabet, who collaborated with scientists at CPMC’s Research Institute, the University Duisburg-Essen in Germany and the Knight Cancer Institute in Portland, OR for the study.
Epidemiological studies suggest a role for UVR in melanoma causation, supported by whole genome sequencing studies demonstrating a high burden of UV-signature mutations. But the precise molecular mechanisms by which melanoma develops following UVR remain poorly understood, necessitating the identification of additional molecular factors that govern both UV and melanoma susceptibility.
NCOA3 (also known as AIB1 or SRC-3) is a member of the nuclear hormone receptor coactivator family, and regulates gene expression through its interaction with various transcription factors. NCOA3 was initially shown to be amplified in breast cancer, and has a demonstrated oncogenic role in various solid tumors. However, a role for NCOA3 in UVR-mediated melanomagenesis has not been previously demonstrated.
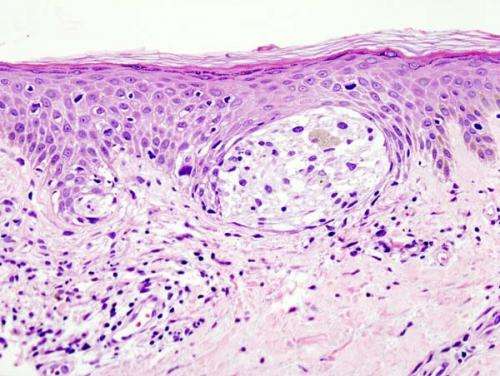
By utilizing a combination of in vitro, in vivo and PDX modeling of melanomagenesis, Dr. Kashani and colleagues assessed the effects of regulating NCOA3 expression in human melanoma cells as well as in melanocytes, identifying multiple oncogenic pathways regulated by NCOA3 in melanoma progression.
Results showed that down-regulation of NCOA3 expression, either by genetic silencing or small molecule inhibition, significantly suppressed melanoma proliferation in melanoma cell lines and PDXs. NCOA3 silencing suppressed expression of xeroderma pigmentosum C and increased melanoma cell sensitivity to UVR. Suppression of NCOA3 expression led to activation of DDR effectors and reduced expression of cyclin B1, resulting in G2/M arrest and mitotic catastrophe.
A single nucleotide polymorphism in NCOA3 (T960T) was associated with decreased melanoma risk, given a significantly lower prevalence in a familial melanoma cohort than in a control cohort without cancer. Additional studies suggest this polymorphism decreases NCOA3 protein production, and is accompanied by increased sensitivity to ultraviolet light—resulting in cell death.
Taken together, these findings are consistent with a model of melanoma initiation whereby elevated NCOA3 expression promotes melanocyte survival following exposure to UVR. This survival advantage enables accumulation of UVR-mediated DNA damage. Over the lifetime of an individual who is susceptible to melanoma, significant exposure to UVR can result in both the high mutational burden and uncontrolled cellular proliferation that characterize the disease. By contrast, these effects are attenuated following expression of the T960T polymorphism, with increased sensitivity to UV-mediated cell death, thereby protecting against the carcinogenic effects of UVR.
“Our results demonstrate an unprecedented role for a molecular marker in distinct stages of tumor progression. These results identify NCOA3 as a candidate susceptibility marker for melanoma, as a potential diagnostic marker, as a prognostic marker of melanoma survival and as a target for therapy. We propose a critical role for NCOA3 in UVR-mediated melanomagenesis, and as a rational therapeutic target for melanoma,” says Dr. Kashani-Sabet.
Skin cancer is the most common type of cancer worldwide. Melanoma accounts for about 1% of skin cancers but causes a large majority of skin cancer deaths. This year, approximately 106,000 Americans will be diagnosed with melanoma.
Source: Read Full Article