Study hints at the promise of non-hallucinogenic LSD for treating mood disorders


Mood disorders are mental health conditions characterized by persistently dysregulated moods, such as recurring feelings of depression or euphoria. According to statistics by the National Institutes of Health, approximately 1 in 5 people in the United States will experience mood disorders at some point in their life.
Given their high incidence and their highly debilitating effects, identifying effective treatments for these disorders is of utmost importance. While there are now countless antidepressant medications on the market, patients tend to respond to each of them differently and some also cause undesirable side effects.
Neuroscientists and pharmacology experts are thus continuously trying to identify alternative pharmacological treatments that might alleviate symptoms of mood disorders with minimal side effects. In recent years, some research teams have been particularly exploring the therapeutic potential of lysergic acid diethylamide (LSD), a psychedelic drug that typically causes hallucinations, as well as intensified emotions and perceptions.
Researchers at Carleton University, BetterLife Pharma Inc., the Medical College of Wisconsin and University of California San Diego (UCSD) have recently carried out a study exploring the potential of a non-hallucinogenic version of LSD for treating mood disorders. Their findings, published in Cell Reports, suggest that non-hallucinogenic LSD could have positive effects of mood, while also reducing the need for medical supervision while taking the drug.
“Since my lab started, we have been working on elucidating the mechanism of action of ketamine as an antidepressant and have a standing interest in identifying new potential treatments for mood disorders,” Dr. Argel Aguilar Valles, co-lead author of the paper, told Medical Xpress. “In the winter of 2021, I was contacted by BetterLife Pharma to collaborate with them in demonstrating the potential of 2-Br-LSD to increase neuronal plasticity and induce behavior in mice that are relevant for antidepressant therapies.”
The recent paper published in Cell Reports was a collective research effort involving separate experiments conducted at Medical College of Wisconsin, Carleton University, and UCSD. These distinct experiments were all aimed at exploring the therapeutic potential and effects of 2-Br-LSD, a non-hallucinogenic analog of LSD created by the pharmacological company BetterLife.
A first research team, led by co-lead author Dr. John McCorvy at Medical College of Wisconsin, specifically tried to identify the pharmacological targets of 2-Br-LSD. This was done using a high-throughput screening platform capable of measuring GPCR activity for over 30 different neurotransmitter receptors and determine whether 2-Br-LSD activated, inhibited or did not affect the activity of each of these receptors.
“It was necessary to test 2-Br-LSD at several molecular targets because LSD interacts with many GPCRs,” Dr. Mc Corvy explained. “We needed to uncover molecular targets that were distinct from LSD to determine what makes 2-Br-LSD non-hallucinogenic and why it is capable of therapeutic potential and worthy of further testing in vivo.”
A second team of researchers led by Dr. Adam Halberstadt at UCSD tested whether 2-Br-LSD induced the so-called head twitch response (HTR) in mice. As suggested by its name, this is a rapid side-to-side head movement typically observed in mice while they are under the influence of psychedelic drugs, including conventional hallucinogenic LSD, but not after consuming non-hallucinogenic analogs.
“While LSD induced the HTR in our studies, 2-Br-LSD did not induce any head twitches even after administration of relatively high doses, which supports the classification of 2-Br-LSD as a non-hallucinogenic 5-HT2A agonist,” Dr. Halberstadt said. “That is a key finding because what is really novel about 2-Br-LSD is that it may mimic some of the therapeutic-like effects of LSD despite being non-hallucinogenic. Therefore, it is important to generate data confirming that 2-Br-LSD doesn’t act as a hallucinogen.”
In addition to not causing the HTR in mice, 2-Br-LSD activated the 5-HT2A receptor (i.e., the primary target of psychedelic drugs) in the mice brain to a lesser extent than hallucinogenic LSD. This weaker activation could potentially explain why this analog drug does not produce hallucinations in humans and HTR in mice.
“Nevertheless, 2-Br-LSD is still active at 5-HT2A and seems to retain enough activity to potentially induce therapeutic effects,” Dr. Halberstadt explained.
Drs. McCorvy, Halberstadt and his colleagues also found that 2-Br-LSD did not activate the 5-HT2B receptor, also known as serotonin receptor 2B. This is a receptor located in several areas of the peripheral and central nervous system, which has been linked to cardiac function.
“5-HT2B activation can be a problem because over time it can damage the valves in the heart, which is why the anorectic drug fenfluramine was taken off the market,” Dr. Halberstadt said. “While LSD acts as a potent 5-HT2B agonist, we found that 2-Br-LSD is not active at 5-HT2B, meaning it may have less potential to produce cardiac side-effects.”
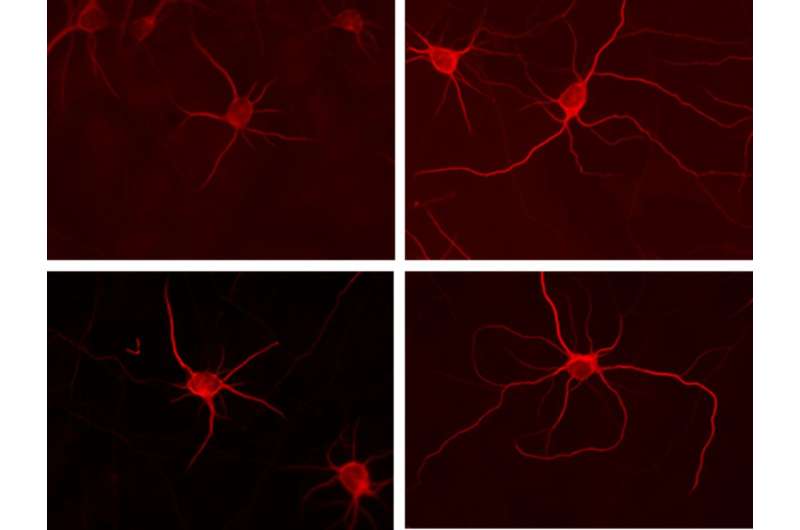
Ultimately, the research group led by Dr. Aguilar Valles at Carleton University carried out a series of experiments on cultured neurons and living mice, to test the effects of 2-Br-LSD on mood. Firstly, they collected measurements to determine whether 2-Br-LSD increased the morphological complexity of cultured rat neurons. Morphological complexity is a measure of neuronal plasticity, or in other words the brain’s ability to change the function, structure and organization of neurons over time.
“We then measured stress-coping behavior in mice and demonstrated that 2-Br-LSD, similar to other effective antidepressants, increased active stress-coping behaviors and reversed the effects of chronic stress, a key risk factor for depression and other mood disorders,” Dr. Aguilar Valles explained. “We also demonstrated that activation of one of the identified 2-Br-LSD receptors (the serotonin receptor 5HT2A) is required for 2-Br-LSD to induce these effects (on cultured neurons and in mouse behavior).”
The findings gathered by Drs. Aguilar Valles, Halberstadt, McCorvy and their colleagues suggest that the pharmacological profile of 2-Br-LSD is far more specific and desirable for the treatment of mood disorders than that of its hallucinogenic counterpart. In addition, the targeted action of 2-Br-LSD on receptors could reduce the risk of undesirable side effects on the cardiac system that some studies linked with the consumption of conventional, hallucinogenic LSD.
“The work of co-lead Dr. Adam Halberstadt confirmed that 2-Br-LSD is not hallucinogenic, as also indicated by studies on humans,” Aguilar Valles said.
“If proven safe and effective in treating mood disorders in human patients, non-hallucinogenic derivatives of serotonergic psychedelic drugs could be used more widely than their hallucinogenic counterparts for therapeutic purposes, because they may require less clinical supervision.”
Overall, the results of this collaborative research effort suggest that non-hallucinogenic LSD analogs, and particularly 2-Br-LSD, could be promising treatments for mood disorders. In addition, the researchers found that they could potentially also serve as anxiolytics, drugs to ease feelings of anxiety.
Before these drugs can be used on human patients, however, they will need to undergo clinical trials on humans to verify their safety and effectiveness. In the meantime, Dr. Aguilar Valles and his lab will continue exploring the neuronal mechanisms underlying the functioning of non-hallucinogenic LSD, as well as other potentially viable antidepressant treatments.
“We want to continue our work on the neuronal mechanisms that this type of drug activates and compare them with the effects of other proven effective antidepressants,” Dr. Aguilar Valles added. “We hope to identify markers or mechanisms shared by drugs with similar antidepressant profiles, so that we can improve our screening process of potential pharmacotherapies for mood disorders.”
More information:
Vern Lewis et al, A non-hallucinogenic LSD analog with therapeutic potential for mood disorders, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.112203
Journal information:
Cell Reports
Source: Read Full Article