‘Smart’ bandages could help with wound care

Around 7 million people in the U.S. suffer from chronic wounds that don’t heal as they should, costing billions of dollars per year in health care costs to treat them—not to mention the human cost to patients’ well-being.
New research from Binghamton University’s Thomas J. Watson College of Engineering and Applied Science takes an initial step toward better understanding of the wound-healing process through “smart” bandages.
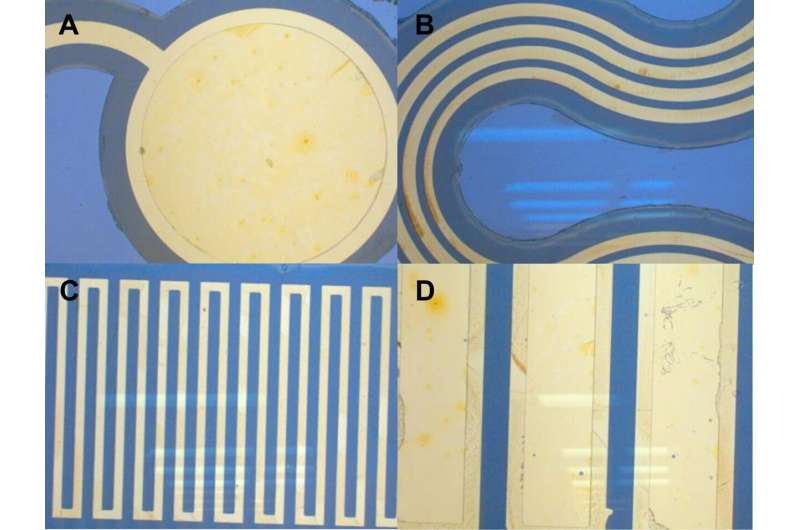
In a paper published in ACS Sensors, Matthew Brown, Ph.D., and Assistant Professor Ahyeon Koh from the Department of Biomedical Engineering propose an adhesive-free, stretchable and permeable wound-care platform that would feature multiple sensors to offer real-time data about exudate (the medical term for wound discharge). A heating element also would keep wounds at an optimum temperature.
Other collaborators in the research were Karen Browne, clinical instructor at Binghamton’s Decker College of Nursing and Health Sciences, and Nancy Kirchner, a nurse specializing in wound care at UHS Wilson Medical Center in Johnson City. A UHS collaboration fund and Watson College’s research seed fund provided financial support.
“We wanted it to be used specifically for wound-care monitoring, where it potentially could be beneficial with those kinds of high-risk patients,” Brown said. “The adhesive-free properties reduce the risk of skin tears, which happen when a strong adhesive is placed on an open wound and the re-healed tissue is removed along with the adhesive.”
The current medical procedure is for doctors and nurses to inspect wounds to see if there is any visible infection, but that method is far from foolproof—especially with chronic wounds, which get stuck in an inflammatory phase and never close properly.
“There’s a lack of quantitative analysis in these types of wounds, and we hope that these technologies can help address that issue,” Brown said. “Looking at real-time analytics of these inflammatory biomarkers like lactate, glucose, oxygen levels or pH could help us better understand how these wounds progress.”
Brown—who now works for Dexcom, which manufactures continuous glucose monitors—sees this research as the culmination of his Ph.D. work at Binghamton, which included better material for wearable biosensors and a process to turn old CDs into sensors.
However, both he and Koh acknowledge that more research is needed before smart bandages are available in hospitals or to the general public. Testing under laboratory conditions clearly is different from treating patients using the information that the devices provide.
Source: Read Full Article