Scientists develop pseudo cell formulation for vitreoretinal disease therapy
Researchers from the Institute of Process Engineering (IPE) of the Chinese Academy of Sciences and Beijing Chaoyang Hospital have developed a new “pseudo cell” formulation based on self-healing microcapsule-loading exosomes to treat diverse vitreoretinal diseases.
The study was published in Nature Biomedical Engineering on Oct. 23.
Vitreoretinal diseases include a wide spectrum of vision-threatening disorders, which may cause severe irreversible vision loss. The efficacy of current treatments for vitreoretinal diseases in clinic is generally unsatisfactory and treatments often cause several side effects. Moreover, frequently repeated treatments are often needed, leading to poor patient compliance.
In recent years, researchers have explored the possibility of cell-based therapy in ophthalmology. Despite some positive results, cell-based therapeutics in ophthalmology have encountered a series of problems, such as low cell-survival rates, instability of cell phenotype and the need for strict storage conditions, which have limited the clinical feasibility of these cell-based technologies.
The therapeutic benefits of many cell types are known to involve paracrine mechanisms. Therefore, researchers have explored the possibility of using more stable cell-secreting components (such as exosomes) as therapeutic components to treat ocular diseases. Inspired by this, researchers from IPE and Beijing Chaoyang Hospital have proposed a “pseudo cell” formulation platform.
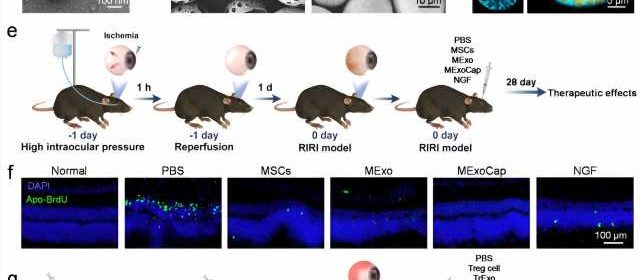
In this platform, exosomes isolated from cells were loaded into self-healing microcapsules, called ExoCaps. “ExoCaps simulate functional cells in terms of size, internal structure, and secretion behavior,” said Prof. Ma Guanghui from IPE.
After intravitreal injection, ExoCaps settled in the inferior area of the vitreous cavity. Since blurred vision can be induced by suspension of living cells in the vitreous cavity, having the ExoCaps settle in the inferior area made it possible to avoid blurry vision. Moreover, exosomes were gradually released as the microcapsules degraded over a month, paving the way for a long-term therapeutic effect.
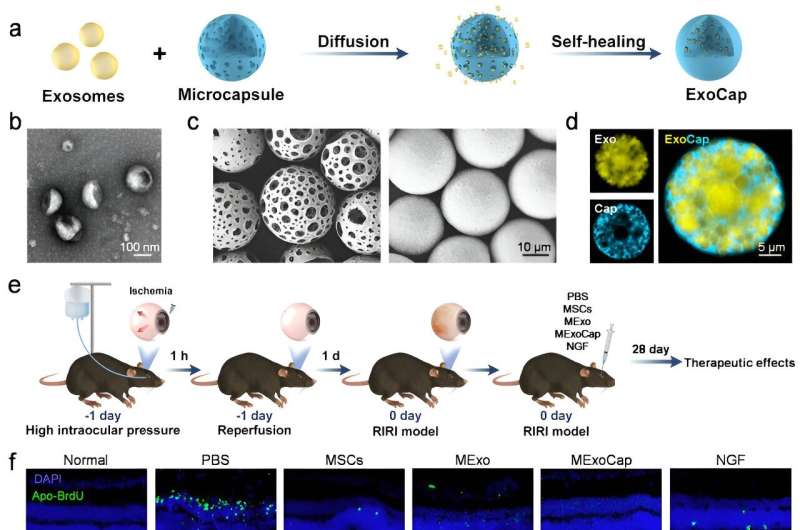
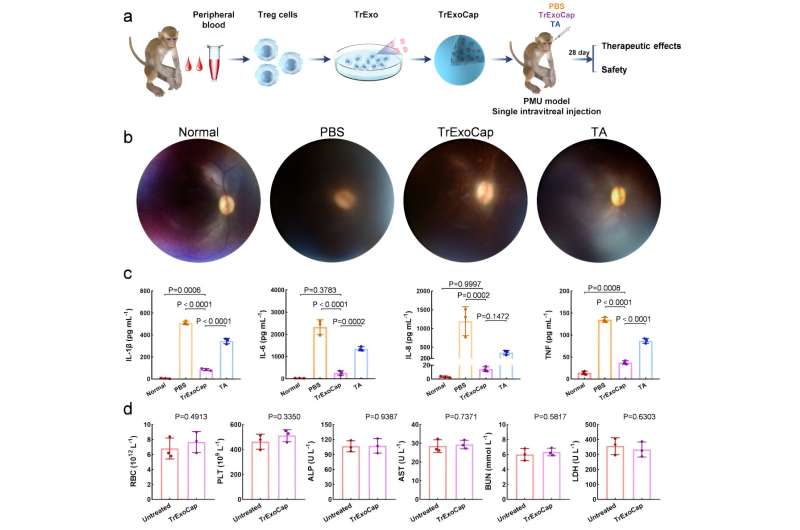
Using retinal ischemia-reperfusion injury (RIRI) and primed mycobacterial uveitis (PMU) models, the researchers detected therapeutic benefits from the application of two different ExoCap formulations, based on microencapsulation of mesenchymal stem cell-derived exosomes (MExo) and Treg cell-derived exosomes (TrExo), respectively. “Our ExoCap platform is flexible and can load exosomes of different cellular origins to meet varied therapeutic needs,” said Prof. Wei Wei from IPE.
The potent therapeutic efficacies were verified in both murine and nonhuman primate models of vitreoretinal diseases. “This study is still at the preclinical stage. Given that exosomes are natural vesicles produced from endogenous cells with good biocompatibility and the microcapsule material [poly(lactic-co-glycolic acid)] has been approved for clinical use, ExoCap has the potential for translation to the clinic,” said Prof. Tao Yong from Beijing Chaoyang Hospital.
More information:
Exosome-loaded degradable polymeric microcapsules for the treatment of vitreoretinal diseases, Nature Biomedical Engineering (2023). DOI: 10.1038/s41551-023-01112-3
Journal information:
Nature Biomedical Engineering
Source: Read Full Article