Researchers uncover mechanisms of brexanolone and the role of inflammation in post-partum depression
Post-partum depression (PPD) develops after childbirth and affects both the mother’s and the infant’s health by preventing healthy bonding. Women with PPD experience intense anxiety, feelings of depression, sleeplessness, inability to care for their child, and risk for suicide.
Brexanolone, an IV infusion comprised of a derivative of progesterone, was approved by the U.S. Food and Drug Administration for the treatment of PPD in 2019. The fast-acting medication significantly reduces depression symptoms and provides effects for up to 90 days. However, exactly how the drug provides these therapeutic effects has remained a mystery—until now.
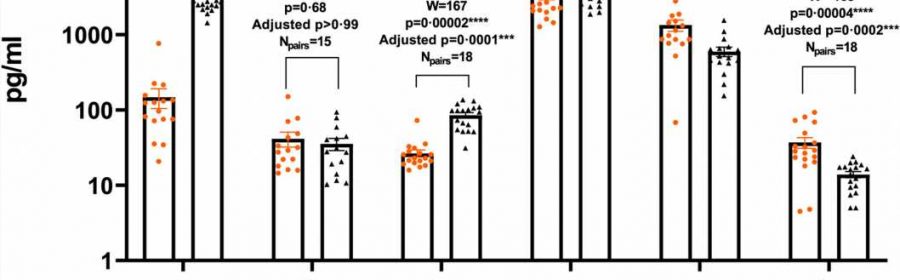
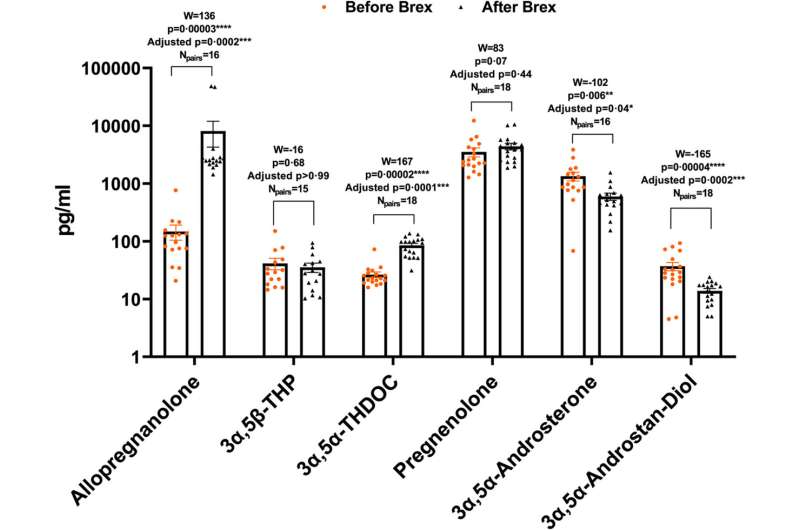
A research team led by A. Leslie Morrow, Ph.D., the John Andrews Distinguished Professor of Psychiatry and Pharmacology in the UNC School of Medicine, has found that brexanolone works within the body by inhibiting the key systemic inflammatory pathways that are associated with depression. The new finding is monumental in that it suggests that PPD is likely caused, at least in part, by inflammation.
“We found that brexanolone inhibited the toll-like receptors responsible for the production of cytokines and chemokines—the markers of inflammation,” said Morrow. Toll-like receptors are like gatekeepers on the surface of cells, recognizing molecules and then initiating a cell’s inflammatory response. “Our results provide the first human data showing that blockade of specific inflammatory pathways is likely involved, at least in women who were unresponsive to other medications.”
Their results were published in eBioMedicine.
According to recent studies, one in eight women experience post-partum depression symptoms, and the prevalence of depression diagnoses at delivery is rising. The CDC reports that rates in 2015 were seven times higher than they were in 2000.
However, scientists are still unsure of what causes PPD to develop in the brain.
One potential cause of PPD could be deficiency in GABAergic transmission, which calms the brain via a neurotransmitter known as GABA. GABA, or y-Aminobutyric acid, is found in our central nervous systems and instructs our bodies to stop, or inhibit, the activity of neurons. Additionally, PPD could also be caused by deficits in our normal responses to stress.
But recent data and this new study suggest that inflammation may be contributing to the syndrome.
Much like other types of depression, PPD is typically treated with SSRIs, but sometimes patients don’t improve with to conventional therapy. Now, doctors are able to prescribe brexanolone in such circumstances. Brexanolone was initially approved in 2019, but the mechanism underlying its antidepressant action was unclear at the time.
The research suggests that the therapeutic effects of brexanolone are likely brought on by its ability to inhibit toll-like receptor pathways and reduce inflammatory markers. The same inflammatory markers have been shown to be up-regulated in PPD, which means that inflammation may be at least partially responsible for the condition.
By the same reasoning, brexanolone or other anti-inflammatory drugs may also be effective for treating other types of depression that elevate inflammatory markers. The team hopes that their new findings may lead to more cost-effective treatments that can block the same inflammatory pathways that were identified in the study.
More information:
Irina Balan et al, Brexanolone therapeutics in post-partum depression involves inhibition of systemic inflammatory pathways, eBioMedicine (2023). DOI: 10.1016/j.ebiom.2023.104473
Journal information:
EBioMedicine
Source: Read Full Article