Researchers link immune-cell activity to psychiatric symptoms in women with HIV

Women with HIV frequently experience neuropsychiatric disorders such as depression, anxiety, and even cognitive impairment. Until now, though, the disordered physiological mechanisms underlying such symptoms was unclear.
A study by a team that includes a Johns Hopkins statistician concludes that at least part of the answer lies in patients’ T-cells, those special white blood cells that are part of the human immune system.
“We found that activation of certain T-cells was beneficial and associated with improved attention and memory, but that activation of other T-cells was associated with more depressive and other symptoms,” said study co-author Yanxun Xu, an associate professor in the Department of Applied Mathematics and Statistics at the Whiting School of Engineering. “Understanding this link offers the opportunity to develop treatments that could prevent these neuropsychiatric complications from occurring in the first place.”
The team’s results appear in the November issue of Brain, Behavior & Immunity—Health.
Xu and graduate student Yuezhe Wang provided statistical analysis for the study, which was led by Leah Rubin, associate professor of neurology at Johns Hopkins Medicine.
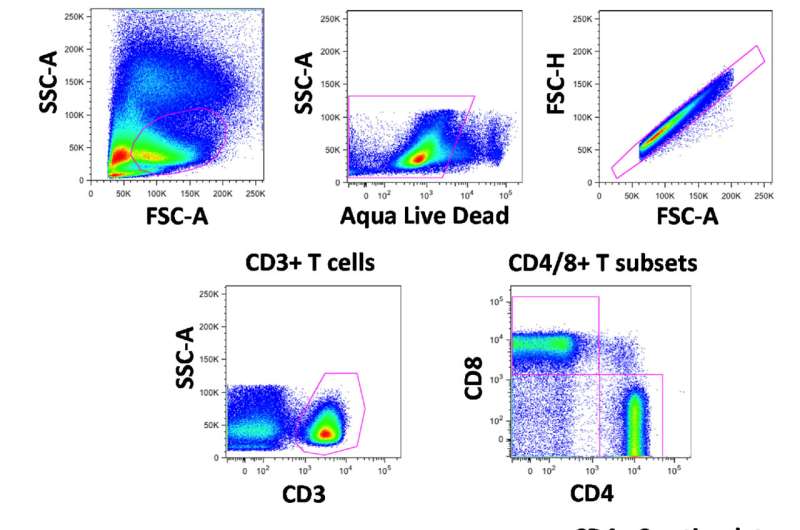
Using a statistical/machine-learning approach called “partial least squares regression” or PLSR, they examined associations between various T-cell phenotypes and neuropsychiatric outcomes in women with HIV.
Xu said that PLSR was the ideal method for the task at hand because it can assess the relationship between multiple outcomes—in this case, neuropsychiatric symptoms—and multiple predictors—in this case, T-cell activation states. (Activation states include a series of activity involving the cells, including when they are stimulated and functioning normally, as well as when they are exhausted and aging.)
“In this research project, the outcomes consist of cognitive assessments of seven domains, including learning, memory, executive function, fluency, attention/working memory, processing speed, and motor function, and self-reported neuropsychiatric outcomes including depressive symptoms, stress and PTSD. The predictors include eight variables assessing T-cell phenotypes,” she said.
Specifically, the study found that patients whose CD4+ T-cells were activated had better working memories and attention spans. But when those patients’ CD4+ T-cells were exhausted (meaning they had lost or diminished ability to kill virus-infected cells), the patients not only had difficulty with working memory and attention, but also showed symptoms of depression. The same was true of patients whose CD8+ T-cells were activated: They had depressive symptoms, as well as exhibited weaker executive function (a set of self-regulation skills, including planning.)
“This is important to know and understand because HIV is now considered a chronic disease and care is mostly focused on better managing long-term, adverse effects, such as cognitive impairment and mental health disorders,” Xu explained.
Xu, who also serves as an adjunct associate professor in the Division of Biostatistics and Bioinformatics at Johns Hopkins’ Sidney Kimmel Comprehensive Cancer Center, has been involved in research related to HIV since 2018, when she began her collaboration with Rubin. Her work focuses on developing novel statistical and machine learning approaches for understanding the effects of antiretroviral drugs on people’s health outcomes and facilitating precision medicine in HIV.
“Optimizing sequential combination antiretroviral treatments over a long-time span tailored to individuals’ evolving clinical characteristics and treatment histories is important for improving long-term health and quality of life for people with HIV,” she said.
Source: Read Full Article