New study brings personalized immunotherapy prescriptions a step closer

In a step likely to advance personalized cancer treatment, scientists have—for the first time—shown in patients that levels of biomarkers are not enough to tell which patients are likely to respond best to immunotherapy.
Instead, clinicians need to understand how immune cells and tumors are interacting within a patient, rather than simply the levels of each associated protein present, to prescribe the best treatment.
The research team, from the University of Bath’s Centre for Therapeutic Innovation (CTI-Bath) alongside colleagues in Bordeaux, France, have published the study in the journal Cancers as a featured article.
The results validate a quantitative imaging platform used at CTI-Bath that can predict whether a cancer patient would respond to immunotherapy treatment.
Cancers evade detection by the immune system, making themselves invisible to the natural anti-tumor response and actively blocking it. One type of immunotherapy, called immune checkpoint inhibitors, involves antibodies that remove the brakes that the tumor has applied to the immune system. This re-activates the patients’ natural anti-cancer response, which then destroys the tumor.
Currently, clinicians use commercial methods to determine levels of immune checkpoint regulators (proteins) within patients to evaluate whether immunotherapy is needed. However, not all patients respond well and the therapy can have serious side effects, so a more refined way to identify which patients will benefit from the treatment is crucial.
To investigate the role of these types of the immune checkpoint regulators in cancer patients, the research team from the Bergonie Cancer Institute (Bordeaux France) and University of Bath professors Banafshe Larijani (Director of the Centre for Therapeutic Innovation (CTI-Bath) and Stephen Ward (Professor of Leukocyte Biology) recruited patients with metastatic lung tumors who were undergoing a treatment called radiofrequency ablation (RFA) at Bergonie Cancer Institute.
In some cases, treating tumors in one lung using RFA can cause tumors in the other lung to also reduce in size. This effect is thought to be due to the cancer treatment provoking an anti-tumor immune response, but can be limited by the interactions of the immune checkpoint regulators. In this process the proteins interact like a lock and key, with regulator proteins entering their immune system protein targets and closing them—thus compromising the immune response.
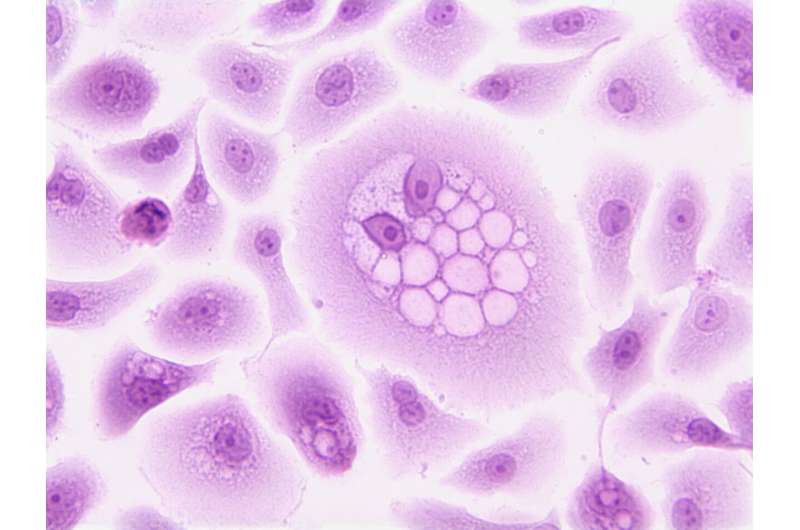
The researchers compared levels of these regulators and their targets with how they were actually interacting—the level of “engagement” (and therefore their activation state)—using the immune-FRET molecular imaging platform developed by Professor Larijani and co-workers in UK and the EU. iFRET can establish how molecules interact at a nanoscale level in single cells and tissue samples.
This is the first time these interactions have been quantified within RFA patients, and they show that engagement did not correlate with the quantity of protein present—meaning that the prescribing based on the levels of proteins present is unlikely to be suitable.
Professor Banafshe Larijani said, “These results show that you can get a better picture of what’s happening within a patient by measuring engagement of immune checkpoint interactions, thus more accurately predicting level of immune suppression and likely response to RFA treatment, instead of simply the levels of the proteins involved. Ultimately we hope this can result in a change in how immunotherapy is prescribed to RFA patients so it’s personalized to an individual.
“Moreover, we’re delighted that the study shows iFRET provides a method for advanced quantitative immune surveyance—as opposed to qualitative immune surveyance—of patients, which will greatly increase patient access to precision medicine.”
Professor Stephen Ward added, “This work emphasizes the importance of developing personalized approaches to cancer therapies that are more targeted and thus likely to be more effective. This is beneficial not just to patients who will receive treatments most likely to work for them, but also to the NHS, and other health services, which will be more efficient in terms of both positive patient outcome and treatment costs.”
Source: Read Full Article