Highlighting the struggle that breastfeeding women experience around the globe

A Lancet Series published on Feb. 8, 2023, highlights the continuing struggle that women across the globe face to meet their breastfeeding goals. Yale School of Public Health Professor Rafael Pérez-Escamilla, a leading authority on breastfeeding and early childhood nutrition, is co-author of all three Series articles and the lead author of the first paper featured in the Series.
The article entitled, “Breastfeeding: crucially important, but increasingly challenged in a market-driven world,” examines how mother and baby attributes at the individual level interact with breastfeeding determinants at other levels, how these interactions drive breastfeeding outcomes, and what policies and interventions are necessary to achieve optimal breastfeeding.
Findings:
- Commercial milk formula (CMF) products and artificial formula feeding cannot emulate the living and dynamic nature of breastmilk and the human interaction between mother and baby during breastfeeding.
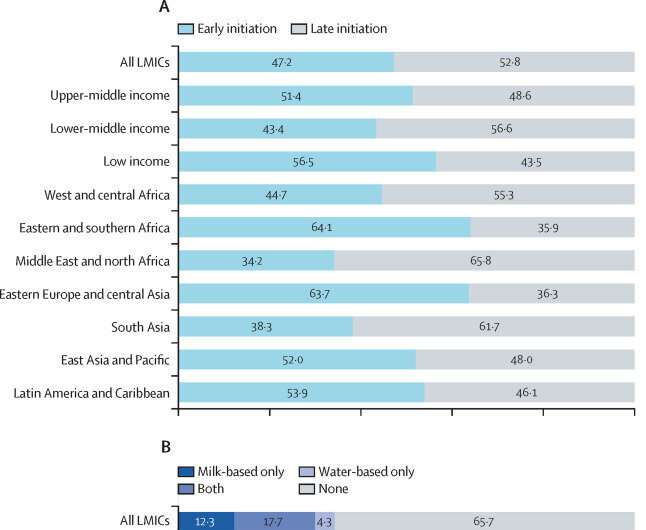
- Only half of newborn babies are put to the breast within the first hour of life, and about a third of babies in low-income and middle-income countries receive prelacteal feeds (mostly water and animal milk) before being put to the breast. Prelacteal feeding is strongly associated with delayed initiation of breastfeeding and shorter breastfeeding duration.
- Common infant adaptations to the post-birth environment, including crying, unsettled behavior, and short night-time sleep durations, are often misconceived as signs of feeding problems. CMF marketing reinforces and exacerbates these misconceptions and makes unsubstantiated claims that CMFs can ameliorate these behaviors.
- Nearly half of mothers globally self-report insufficient milk (SRIM) as the primary reason for introducing CMFs in the first few months of life. SRIM can generally be prevented or addressed successfully with appropriate support.
- Additional educational efforts are needed for health workers, families, and the public to inform them about normal early infant development, including common crying patterns, posseting, and short night-time sleep durations, to reduce the unnecessary introduction of CMFs and to prevent SRIM and early cessation of breastfeeding.
- Breastfeeding is not the sole responsibility of the mother. Reviews and country case studies indicate that improved breastfeeding practices at the population level are achieved through a collective societal approach that includes multilevel and multicomponent interventions across the socioecological model and different settings.
Professor Pérez-Escamilla took a moment to expound on the findings.
This latest Series published by The Lancet follows up on an initial breastfeeding Series that was published in 2016. What has changed since then and are global breastfeeding rates improving?
P-E: On the one hand, evidence has continued to accumulate showing that breastmilk not only provides optimal nutrition to infants but is also loaded with bioactive substances that protect the child against infectious and non-infectious diseases. The composition of breastmilk is unique to the needs of each infant in the environment in which the child grows.
So, in many ways, we now have irrefutable evidence that breastfeeding is Mother Nature’s expression of personalized medicine. Furthermore, in the Series, we present evidence from innovative research showing that breastfeeding protects against the risk of childhood obesity in low and middle-income countries (LMICs) and not only in high-income countries (HICs).
Regarding breastfeeding programs, the Series provides new evidence showing that in countries where exclusive breastfeeding rates have increased in recent years—such as Mexico, Mozambique, the Philippines, and the U.S.—this has been the result of investments in multilevel and multisectoral interventions ranging from improved maternity benefits for employed mothers to social and behavior change communication campaigns to improved coverage of the Baby Friendly Hospital Initiative and breastfeeding counseling across clinical and community settings.
Not all women wish to breastfeed or can breastfeed for a variety of reasons. Yet not all commercial milk formulas offer the same levels of nutrition. What can be done to help mothers make sure their children are getting the important nutrition they need?
P-E: The Series fully acknowledges that women have the right to choose how to feed their infants and that choice should be respected and supported no matter what. If women chose to not breastfeed or to mix feed, or cannot breastfeed, of course, infant formula is the milk product that should be offered during the first year of life and at that point, infants should switch to regular cow’s milk. The Series clearly shows that, contrary to what CMF marketing often implies, there is no need for the quite expensive toddler milks marketed for children between 1 and 3 years old.
Milks based on plant protein sources such as soybeans are also available for the few infants and young children that do not tolerate cow’s milk, but this decision needs to be made in close consultation with a qualified health provider.
It is important to emphasize that the Series is not a manifesto against infant formula (a product that is vital for infants who are not breastfed), but rather a call to decision-makers and authorities to stop infant formula companies from undermining mothers’ breastfeeding intentions through misleading marketing that exploits their fears and emotions during a very vulnerable period.
You mention that normal baby behaviors like crying are often misconstrued and can lead a mother to stop breastfeeding. Can you elaborate on this point and share what interventions may help in these cases?
P-E: Infant crying is part of normal infant development; this is indeed how babies communicate their physical and psycho-emotional needs. Understandably, parents can get very worried and distressed when their infants cry. Unfortunately, infant formula companies exploit these psycho-emotional sensitivities of parents by marketing their products as helping babies cry less and sleep better, without evidence to support these claims. In other words, they have found that marketing their products by selling parents “tranquility” and “peace of mind” is very profitable.
Additionally, oftentimes health providers tell parents that the baby is crying frequently because the mother is not producing enough milk and advise them to introduce infant formulas right away without even assessing first the baby’s growth and developmental status. Even more worrisome is the fact that these same providers oftentimes benefit from relationships with infant formula companies that are underlined by clear conflicts of interest.
Babies cry for many reasons including being hungry, cold, hot, tired, or simply because they have a wet diaper, or their environment becomes too loud for them. We have the know-how to train health providers on how to effectively counsel parents and other caregivers on how to understand what their babies are communicating when crying and how to respond to these cues without undermining breastfeeding.
Self-reported insufficient milk is a common reason why mothers stop breastfeeding. You say this can be addressed with appropriate support and health care training. Can you elaborate?
P-E: To prevent the pervasive maternal report of insufficient milk, it is important to provide anticipatory guidance to mothers on what to expect with breastfeeding once the baby is born.
If the mother wants to breastfeed, she should request that her newborn be placed skin-to-skin with her immediately after birth and she should let care providers know she wants to initiate breastfeeding as soon as possible. If the mother has not breastfed before, she should ask for a lactation counselor to observe the baby’s latch as many problems with breastfeeding happen during the first hours and days after birth because of poor positioning.
New moms should also be advised that it takes about 3 days for the milk to “come in” and that she needs to breastfeed the baby on demand, and to not agree for the baby to be fed formula in the maternity facility unless it is medically indicated. This is because breastmilk production is a process driven by infant sucking and any interference with the frequency of nursing increases the risk of breastfeeding failure.
It is also very important to counsel mothers on how to interpret normal baby behaviors such as crying and “disorganized” sleep routines during the early neonatal period, and how to respond accordingly without negatively affecting their breastfeeding plans. It is also key to include partners or other family members or friends as part of these counseling sessions as, not surprisingly, they also have the widespread belief that infant crying is always a sign that moms are not producing enough milk.
And lastly, maternity facilities and community providers should coordinate their breastfeeding support services following a continuum of care approach so that all mothers can have access to qualified lactation management services no matter where they are, especially during the first days and weeks after hospital discharge, which is when most breastfeeding crises happen and need to be prevented or resolved.
Lastly, you point out that breastfeeding is not solely a mother’s responsibility but that population-level interventions can help improve global breastfeeding rates. What do you mean, and can you give us examples of these interventions?
P-E: Globally, the great majority of women are choosing to breastfeed but unfortunately most of them cannot breastfeed for as long as they would like due to major social, political, economic, and health care structural barriers. This represents a major violation of women’s and children’s rights that strongly undermines global health and national development globally.
The Lancet Series nicely integrates new evidence showing how important it is for all of society to support the wishes of breastfeeding mothers through (1) social protection policies (e.g., improved maternity benefits for women working in the formal and informal economy; workplace accommodations including lactation rooms, and flexible working schedules); (2) marketing regulation (implementation and strong enforcement of the World Health Organization Code for Marketing of Breastmilk Substitutes)); (3) social and behavior change communication campaigns to support breastfeeding moms anytime and anywhere; (4) health care systems programs such as the Baby Friendly Hospital Initiative; (5) breastfeeding counseling in community settings; (6) access to human milk banks; and (7) support from family and friends for breastfeeding including support with household chores and caregiving of the baby and siblings.
More information:
Breastfeeding 2023: Series from the Lancet journals. www.thelancet.com/series/Breastfeeding-2023
Journal information:
The Lancet
Source: Read Full Article