Has a treatment for Alzheimer’s been sitting on pharmacy shelves for decades? Scientists have two possible candidates

Two drugs approved decades ago not only counteract brain damage caused by Alzheimer’s disease in animal models, the same therapeutic combination may also improve cognition.
Sounds like a slam dunk in terms of a cure—but not yet. Researchers currently are concentrating on animal studies amid implications that remain explosive: If a surprising drug combination continues to destroy a key feature of the disease, then an effective treatment for Alzheimer’s may have been hiding for decades in plain sight.
A promising series of early studies is highlighting two well known medicine cabinet standbys—gemfibrosil, an old-school cholesterol-lowering drug, and retinoic acid, a vitamin A derivative. Gemfibrosil, is sold as Lopid and while it’s still used, it is not widely prescribed. Doctors now prefer to prescribe statins to lower cholesterol. Retinoic acid has been used in various formulations to treat everything from acne to psoriasis to cancer.
The two drugs are being studied for their robust impact on the brain and a potential new role that could one day thrust them into fighting what is now an incurable brain disease. Both medications have an uncanny capability to zero in on the brain’s astrocytes, cells that originally got their name because they look like stars. But astrocytes are intimately involved in a key process that progressively—and insidiously—destroys the brain.
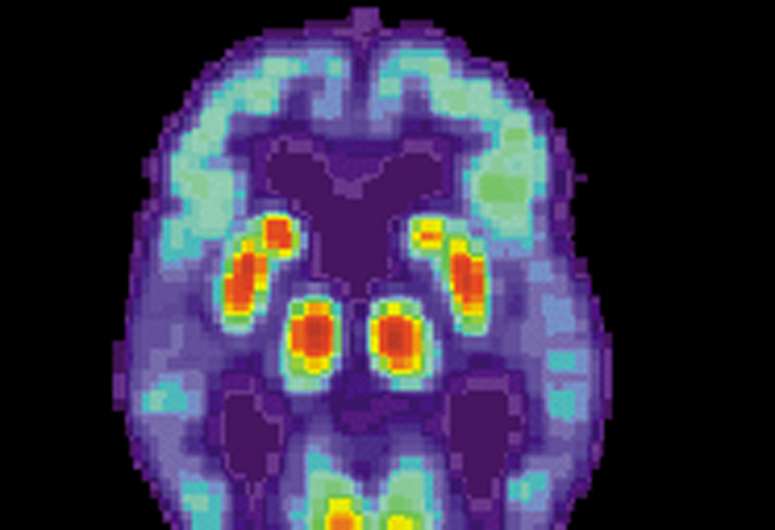
Researchers at Rush University Medical Center in Chicago have found that astrocytes may be responsible for the accumulation of amyloid beta (Aβ), the gooey plaque that damages neurons. As a result, these star-like cells aid in the cascade of deleterious events that rob people of their sense of self, their memories, and ultimately steals their lives.
The team of medical investigators also has discovered that gemfibrozil and retinoic acid, when used in combination, force astrocytes to reverse their destructiveness, and instead reduce amyloid beta in the brain—improving cognitive function. The findings suggest that, perhaps in the not-too-distant future, these drugs can be repurposed to coax astrocytes into a beneficial role, serving as Aβ “clearing machines,” eliminating the accumulation of plaques and preventing Alzheimer’s from unraveling the brain.
“From a therapeutic angle, these results suggest that low-dose [gemfibrozil and retinoic acid]
might be repurposed as a treatment for reducing the plaque burden and improving cognition,” wrote Dr. Sumita Raha, first author of a paper published in Science Translational Medicine.
“Astrocytes are a type of glial cell that are implicated in the buildup of amyloid beta in Alzheimer’s disease,” Raha added about the drug duo. Along with her Rush Medical Center colleagues, the team is proposing that rather than being intricately involved in the promotion of Aβ accumulation “astrocytes could be induced to take up and destroy Aβ fibrils with an orally ingested combination of drugs that are approved for other indications.”
Astrocytes studied in cell cultures and in Alzheimer’s mouse models were stimulated by retinoic acid to phagocytose—destroy Aβ—through the activation of the low-density lipoprotein cholesterol receptor and triggered to subsequently degrade Aβ in lysosomes by the cholesterol-lowering drug gemfibrozil.
Earlier research led by Raha’s colleague, Dr. Kalipada Pahan, also of Rush, and an author of the current study, found that a combination of gemfibrozil and retinoic acid accelerated the formation of lysosomes in mouse brain cells. Lysosomes are the organelles that contain digestive enzymes and are involved in the breakdown of excess or worn-out cell parts. The word organelle means “little organ,” a term for the components in cells with specialized functions, such as the Golgi apparatus or mitochondria.
Raha, Pahan, and colleagues discovered that gemfibrosil and retinoic acid also caused mouse astrocytes to take in more amyloid beta from outside of the cell. Their experiments revealed that the drug combination activated a receptor called PPARα, which encouraged astrocytes to destroy the mind-damaging amyloid, the cause of plaques. PPARα stands for peroxisome proliferator-activated receptor-alpha. PPARα is a transcriptional factor that regulates the expression of genes involved in fatty acid oxidation and is also a major regulator of energy homeostasis. PPARα is critical in the elimination of amyloid beta, Aβ.
Gemfibrosil is an old drug, first patented in the 1968 as a cholesterol reducer. Retinoic-acid-based drugs are even older. For example, Tretinoin, a retinoic acid medication, was patented in 1957. If the gemfibrosil/retinoic acid drug combination ultimately works in humans, then the Chicago-based team will have ushered into use a new treatment made up of two very old medications.
Although the team at Rush University Medical Center is well into its pursuit of the two-drug combination, it’s not yet known when the experiments might advance to a full-blown human clinical trial. Yet, along with identifying a potential two-drug approach to Alzheimer’s disease, the Chicago experiments also have added to the scholarship about the biology of astrocytes in the brain.
Astrocytes, or astroglia, as they are also known, are a type of glial cell, and they dramatically outnumber neurons. Some estimates suggest there is a fivefold difference between the two types of brain cells favoring astrocytes. While neurons are the cells of all higher functions, such as learning and memory, astrocytes play a major role regulating increases in intracellular calcium. Upping intracellular calcium is required to maintain astrocyte-to-astrocyte and astrocyte-to-neuron communication, studies have shown.
Yet as the gemfibrosil/retinoic acid combination evolves as a potential Alzheimer’s therapy, the larger story about drugs to treat Alzheimer’s has been a tale marred by setbacks and disappointments for decades. The most recent involves questions that arose following the approval in June of Biogen’s Aduhelm, a medication that carries a breathtakingly high price tag—$56,000 a year in the United States.
Medical experts voiced concern about studies leading to the drug’s approval. Taken as a whole, the research demonstrated mixed results. But the drug, which is administered as an infusion, was fast-tracked through the U.S. Food and Drug Administration’s authorization process.
Worse, Aduhelm is one of slightly more than a half dozen drugs approved in a quarter century to treat Alzheimer’s, a disease that is rapidly becoming one of the largest health crises on the planet, according to the World Health Organization.
Currently, an estimated 55 million people globally have Alzheimer’s disease, and that number could explode to more than 152 million worldwide by 2050 unless a cure is found.
Source: Read Full Article