Exploring mechanisms of resistance to HIV in people with sickle cell disease

A new analysis supports prior reports that people with sickle cell disease have lower rates of human immunodeficiency virus (HIV) infection, but follow-up cell studies did not reveal a mechanism to explain the reduced risk. Shannon Kelly of Vitalant Research Institute in San Francisco, CA, and colleagues presented these findings in the open-access journal PLOS ONE on April 8, 2020.
A number of epidemiological reports have suggested that people with sickle cell disease experience low rates of HIV infection compared to the general population. However, the mechanisms behind this reduced risk remain unclear. To better understand the reduced risk, Kelly and colleagues conducted a two-part investigation. First, they ran a new statistical analysis of data from a previous study of people with conditions characterized by low red blood cell count, including sickle cell disease. They found that those with sickle cell disease did indeed experience lower rates of HIV infection.
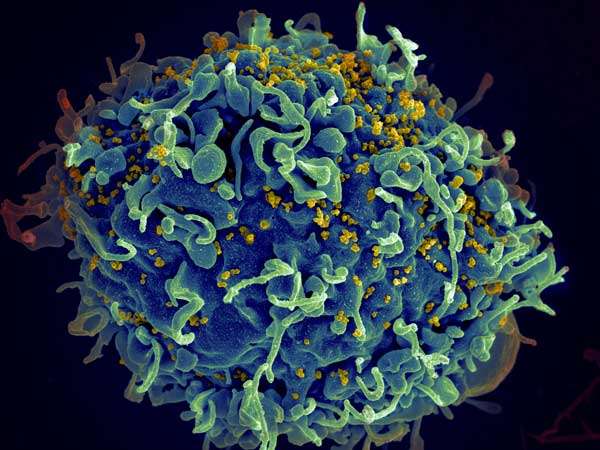
Next, the researchers conducted a lab study of immune system cells isolated from blood samples from HIV-negative patients with or without sickle cell disease. They hypothesized that lower risk of HIV infection might be related to molecular characteristics of immune system cells known as CD4+ T cells.
The lab studies did find that CD4+ T cells from people with sickle cell disease had lower levels of CCR5, a key protein involved in HIV infection. These cells also had lower levels of the protein CCR7 and higher levels of the protein CD4. However, further experiments showed that the cells were no less susceptible to HIV infection than were CD4+ T cells from people without sickle cell disease.
These findings lend further support to the idea that people with sickle cell disease are less likely to be infected with HIV. However, further research is needed to determine whether the molecular differences uncovered in this study are related to this lower risk, or if other mechanisms are at play.
Source: Read Full Article