Experts present detailed evidence on the impact of environmental issues on cardiovascular health
There is already robust evidence that people living with cardiovascular disease are disproportionately affected by poor air quality and extreme temperatures, in large part due to climate change, the greatest threat to human health of the 21st century. In this special theme issue of the Canadian Journal of Cardiology, noted experts comprehensively review how climate change occurs and increases the risk of cardiovascular disease and provide practical tips on how to become a climate-smart cardiovascular health care provider.
Not long ago, climate change was a fringe topic deemed only to affect rare species and ignored by many. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 estimated that nine million people died prematurely because of air pollution in 2019. Nearly 62% of these deaths were related to cardiovascular diseases, highlighting the fact that climate change is not only a general health care issue, but also a major cardiovascular health issue.
This issue of the Canadian Journal of Cardiology is guest-edited by Sadeer Al-Kindi, MD, Houston Methodist DeBakey Heart and Vascular Center; Matthew Bennett, MD, FRCPC, University of British Columbia; Daniel Gagnon, Ph.D., Montreal Heart Institute; Sanjay Rajagopalan, MD, FACC, FAHA, Harrington Heart and Vascular Institute; and François Reeves, MD, FRCPC, University of Montreal.
The Guest Editors explain, “The health effects of heat extremes and poor air quality notably drew attention recently because of the 2021 heat dome that resulted in 619 heat-related deaths in British Columbia, Canada; the European summer of 2022 that was the hottest on record and caused an estimated 61,672 heat-related deaths; and the wildfires in Québec, Canada, that caused poor air quality across vast areas of Northeastern America during the summer of 2023.” Within this context, it has never been more relevant to understand how environmental influences affect cardiovascular health to mitigate their effects.
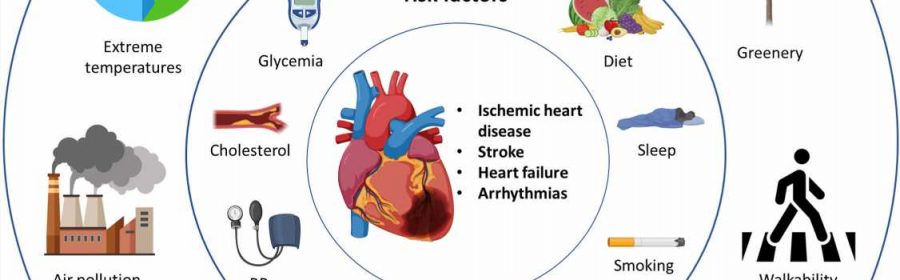
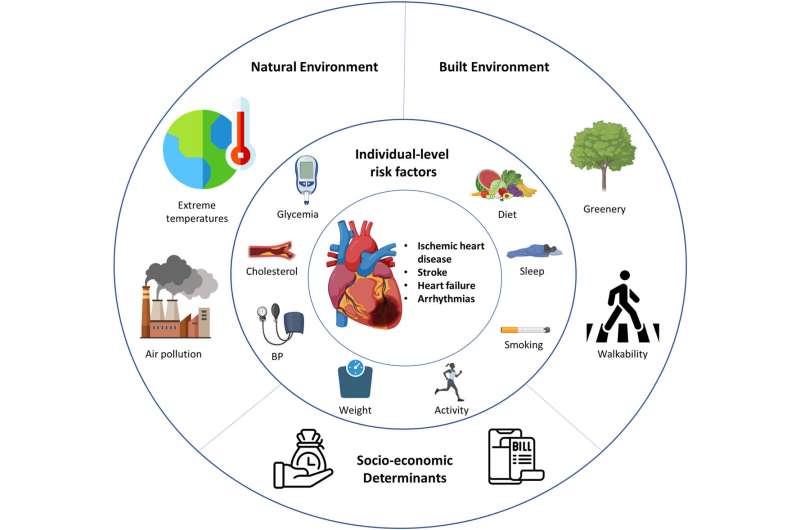
In addition to extreme weather and air pollution being associated with cardiovascular events, it is increasingly recognized that the comprehensive lifetime exposure of individuals and populations to their surrounding environment (the exposome) is closely interlinked to cardiovascular health and well-being.
Issam Motairek, MD, Case Western Reserve University School of Medicine, and colleagues review the relationship between the exposome and cardiovascular health, highlighting the epidemiological and mechanistic evidence of environmental exposures on cardiovascular disease. This review also reinforces the importance of minimizing long-term pollutant exposure for the prevention of cardiovascular disease.
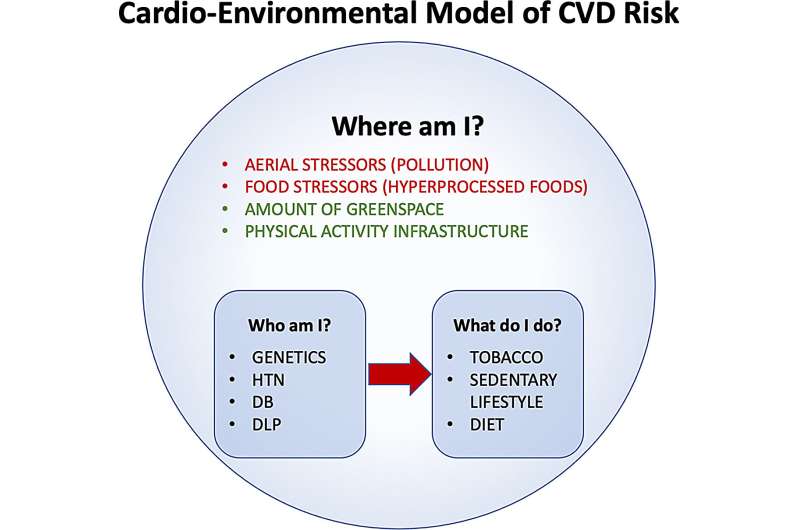
Aerial nano-aggressors (air pollution), food nano-aggressors (hyperprocessed food), the level of greening, and an environment encouraging (or not) physical activity are major environmental determinants of heart health. François Reeves, MD, FRCPC, and Brian J. Potter, MDCM, SM, FRCPC, both of the University of Montreal, propose a cardio-environmental model for cardiovascular risk assessment of easily evaluated factors by asking: (1) Who is my patient? (family history, ethnicity, traditional risk factors, body mass index, and comorbidities); (2) What does my patient do? (eating habits, smoking, drugs, physical activity); and (3) Where does my patient live? (air quality, food quality, urban environment).
A review by Barrak Alahmad, MD, Ph.D., Harvard T.H. Chan School of Public Health, and colleagues shows that climate change and air pollution worsen each other leading to several ecosystem-mediated impacts. They highlight how increases in hot climates as a result of climate change have increased the risk of major air pollution events such as severe wildfires and dust storms and that altered atmospheric chemistry and changing patterns of weather conditions can promote the formation and accumulation of air pollutants, a phenomenon known as the climate penalty.
Extreme heat events, in which temperature and/or humidity are sufficiently elevated to generate health impacts at a population level, are an important consequence of the accelerating climate crisis. Daniel Gagnon, Ph.D., and colleagues describe how the human body interacts with a hot environment during physical activity, summarize current hot weather guidelines for physical activity, and conclude with practical strategies to encourage safe physical activity in hot weather.
David Kaiser MD, MSc, McGill University, and colleagues point out that cardiovascular clinicians and researchers are uniquely placed to help prevent heat wave mortality by identifying patients who are most at risk and using education, referrals, and advocacy to contribute to public health interventions.
Hypertension is responsible for nearly nine million deaths worldwide annually; environmental pollution increases the incidence of hypertension and exacerbates its severity. Environmental aggressors include the adverse vascular effects of air pollution, lack of green spaces, increased risk of infection, lack of physical activity, temperature effects, noise pollution, disturbance of circadian rhythm, and economic disparities such as limited access to health care.
Francisco J. Rios, Ph.D., McGill University Health Centre, and colleagues highlight their crucial impact and how these determinants influence diverse communities. They also address opportunities and challenges for new research to address knowledge gaps in our understanding of the molecular mechanisms through which environmental factors influence development of hypertension and associated cardiovascular disease.
Adverse air quality increases the risk of many cardiovascular diseases including atherosclerosis and, as a result, the incidence of myocardial infarction, stroke, and cardiovascular death. In addition, acute and chronic increases in air pollution increase the risk of atrial and ventricular arrhythmias, heart failure incidence, and heart failure-related hospitalizations.
A review by Matthew Bennett, MD, and colleagues discusses the association between both acute and chronic air pollution exposure and arrhythmia incidence, morbidity and mortality, and the purported pathophysiological mechanisms. They highlight several pathways mediating this association, including increases in inflammation, oxidative stress, mitochondrial and autonomic dysfunction, cardiac structural changes, and altered calcium, potassium, and sodium channel function.
Cavin K. Ward-Caviness, Ph.D., and Wayne E. Cascio, MD, both of the US Environmental Protection Agency, found substantial evidence linking air pollution exposure to heart failure incidence and related hospitalizations. They propose that further studies specifically to identify data gaps will greatly improve our knowledge of the susceptibility of individuals with heart failure and interventions to reduce risks.
The World Health Organization has reported that more than 1.6 million healthy life-years are lost yearly from traffic-related noise in western Europe. Thomas Münzel, MD, University Medical Center Mainz, and colleagues provide an overview of the “so-called” nonauditory cardiovascular health effects of noise, including acute and chronic ischemic heart disease, heart failure, arrhythmia, and stroke. They also provide evidence from translational human and experimental noise studies and discuss maneuvers to mitigate noise effectively.
Khalid Al-Thalji, MD, University of Toronto, and colleagues describe how to incorporate environmental cardiology into medical education to create climate-smart cardiovascular health care providers to minimize the cardiovascular effects of climate change in patients and the general population, improve awareness of these effects, and create climate change advocates within the cardiovascular community.
The Guest Editors comment, “Through the education of cardiovascular health care practitioners, trainees, the public, and policy makers regarding how and to what degree climate change increases the risk of cardiovascular disease, the impact of environmental factors on cardiovascular health can be minimized.”
Aditya Khetan, MD, McMaster University, and Sadeer Al-Kindi, MD, Case Western Reserve University, explain how patients can adapt to environmental risk, and in particular, what recommendations should be given to high-risk patients during “bad air” days and during times of hot or cold temperatures.
The Guest Editors conclude, “The association between climate change and cardiovascular events is clear. Cardiovascular health practitioners, as health care leaders and educators, can play a leading role in minimizing the effect of environmental factors on cardiovascular health. Ongoing and future research will help manage the influence of environmental factors on cardiovascular health to thrive in a warmer planet.”
More information:
CJC Theme Issue: Environmental Determinants of Cardiovascular Disease Pathophysiology and Therapeutics, Canadian Journal of Cardiology (2023). www.onlinecjc.ca/issue/S0828-282X(23)X0010-5
Journal information:
Canadian Journal of Cardiology
Source: Read Full Article