ESMO 2023: Tarlatamab Shows Promise for Small Cell Lung Cancer
MADRID, Spain — Despite the progress seen with the use of immunotherapy in recent years, only modest advances have been made in the field of small cell lung cancer, which represents 15% of all lung cancer diagnoses. Consequently, the positive results from the phase 2 study of tarlatamab in patients with small cell lung cancer (DeLLphi-301 study) have been met with enthusiasm from specialists. The findings were presented at a session held as part of the European Society for Medical Oncology (ESMO) 2023 Congress.
“We are seeing some truly surprising response rates and progression-free survival data. It’s very encouraging, considering the mediocrity of the second-line treatments we are currently using and tolerance is good,” said Jean-Yves Blay, MD, chairman of Unicancer and general director of the Léon Bérard Center in France, at a press conference.
“It’s in phase 2, so we must remain cautious, but this compound is one to watch since we’re still lacking options with this type of cancer,” added Muriel Dahan, MD, research and development director at Unicancer.
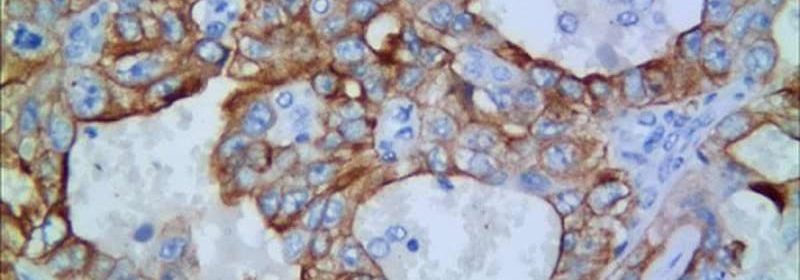
Tarlatamab is a bispecific T-cell engager (BiTE), comprising one part that binds to T lymphocytes and another that binds to cancer cells via the DLL3 receptor, resulting in tumor lysis.
“This bispecific targets an unusual cell surface protein and could be applied to other tumors expressing DLL3, such as neurological and endocrine tumors,” added Blay.
Study Details
In DeLLphi-301, 220 patients with relapsed small cell lung cancer after platinum-based chemotherapy (± checkpoint inhibitor) and at least one other prior treatment line were given 10 mg or 100 mg of tarlatamab once every 2 weeks.
The primary endpoint was objective response as assessed by blinded independent central review (RECIST 1.1). The other endpoints were response duration, progression-free survival, overall survival, and adverse events with onset during treatment.
For a median follow-up of 10.6 months, at a dose of 10 mg, the objective response rate was 40.0%, mean progression-free survival was 4.9 months, mean overall survival was 14.3 months, and mean response duration was not achieved, with 57.5% of participants having a response for 6 months or more and 55.0% still having an ongoing response.
In terms of tolerability, the most common treatment-related side effect was cytokine release syndrome (CRS) (51.1% with 10 mg; 60.9% with 100 mg), which occurred mainly during cycle one, and was mostly scored at grade 1 or 2. The incidence of grade 3 CRS (0.8% with 10 mg; 5.7% with 100 mg) and of grade 3 immune effector cell-associated neurotoxicity syndrome, as well as any related neurologic events, was low (0% with 10 mg; 4.6% with 100 mg), with no grade 4 or 5 events being reported.
Treatment cessation due to side effects was uncommon (3.0% with 10 mg; 3.4% with 100 mg). Similar safety profiles were observed with 24-hour or 48-hour in-hospital monitoring.
“Tarlatamab demonstrated impressive anti-tumor activity with long-lasting responses and promising survival. It showed a favorable risk-benefit profile with no new safety alerts, supporting the use of tarlatamab in patients with small cell lung cancer who are already being treated,” conclude the authors.
In a more general commentary, Blay highlighted that: “During this ESMO [Congress], we have seen the arrival of bispecifics in a number of solid and blood cancers. It’s only speculation at the moment, but they could be an often simpler solution to CAR T-cell or modified T-Cell therapies to achieve the same effect. The findings are very encouraging.”
The DeLLphi-301 study is funded by Amgen.
This article was translated from the Medscape French edition.
Source: Read Full Article