Do Fluoroquinolones Up Risk for Aortic Aneurysm or Dissection?
Previously reported associations between fluoroquinolone use and risk for hospitalization with aortic aneurysm or dissection may be due to confounding, an observational study using two databases and both cohort and crossover designs suggests.
Safety concerns over fluoroquinolones led the US Food and Drug Administration (FDA) to issue a warning in 2018 of an increased risk for aortic aneurysm or dissection with fluoroquinolone use for certain patients. In addition, previous studies have had conflicting results regarding the causality of the associations.
Jeremy P. Brown, MSc, of the London School of Hygiene and Tropical Medicine, United Kingdom, and colleagues write that they used multiple study designs to investigate the associations and “increase the robustness of the findings.”
Published online August 16 in JAMA Cardiology, the study found no association after accounting for potential confounders or when comparing fluoroquinolone use to other antibiotics.
“Our study does provide reassurance to clinicians prescribing fluoroquinolones regarding the risk of this specific outcome,” Brown told theheart.org | Medscape Cardiology.
Confounding a Factor?
The investigators linked Clinical Practice Research Datalink Aurum and GOLD primary care records to hospital admissions data to conduct cohort and crossover studies.
For the cohort study, adults with a systemic fluoroquinolone or cephalosporin prescription between 1997 and 2019 were included. The team estimated the association between fluoroquinolone vs cephalosporin and hospitalization with aortic aneurysm or dissection within 60 days of prescription. Adults with Marfan syndrome were excluded.
In the case-crossover study, adults with a first hospitalization with aortic aneurysm or dissection were included and matched 1:3 to control individuals on age, sex, index date, and clinical practice.
The association between fluoroquinolone prescribing and aortic aneurysm or dissection was assessed relative to nonuse and to comparator antibiotics cephalosporin, co-amoxiclav, and trimethoprim in the 60 days preceding the outcome.
In the cohort study, 3,134,121 adults in Aurum (mean age, 52.5 years; 62.8% women) and 452,086 in GOLD (mean age, 53.9 years; 63.4% women) were prescribed fluoroquinolones or cephalosporins.
In crude analyses, fluoroquinolone relative to cephalosporin use was associated with increased hospitalization with aortic aneurysm or dissection (pooled hazard ratio [HR], 1.28); however, after adjustment for potential confounders, the association vanished (pooled adjusted HR, 1.03).
In the case-crossover study, 84,841 individuals were hospitalized with a first aortic aneurysm or dissection in Aurum (mean age, 75.5 years; 27.8% women) and 10,357 in GOLD (mean age, 75.6 years; 27.1% women).
Relative to nonuse, there was a positive association between fluoroquinolone prescribing and hospitalization with aortic aneurysm or dissection (pooled odds ratio, 1.58). However, the risk also was elevated for comparator antibiotics, and compared with the comparator antibiotics, there was no evidence for an association with fluoroquinolones.
“The results in this study suggest that estimates of association of fluoroquinolones with aortic aneurysm or dissection may be affected by confounding,” the authors write. “When such confounding is accounted for, no association was evident, providing reassurance on the safety of fluoroquinolones with respect to aortic aneurysm or dissection.”
Interpret With Caution
“The findings should be interpreted with caution,” Ismail El-Hamamsy, MD, PhD, Director of Aortic Surgery for the Mount Sinai Health System in New York City, who commented on the findings for theheart.org | Medscape Cardiology. For example, patients with Marfan syndrome or a genetic condition associated with aortic aneurysm, presumably the most vulnerable population, were excluded from this study, he said.
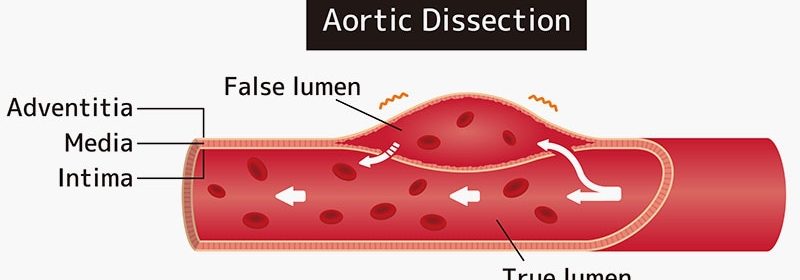
Further, “the outcome of interest was aortic aneurysm or dissection,” El-Hamamsy noted. “A dissection is an acute event and a link to a singular event (antibiotic prescription in the preceding two months) is easier to establish. In contrast, by no means does diagnosing an aneurysm within 60 days suggest that it developed in that time frame,” he said.
“The underlying infection may have simply led to imaging and incidental diagnosis. Therefore, the lack of distinction between aneurysms and dissections is a major limitation of the study.”
Finally, he said, “the study does not address the impact of fluoroquinolones in patients with known aortic aneurysms or connective tissue disorders, which is what the FDA warning is about. Those patients have an inherently higher risk of aortic dissection or rupture. Therefore, for these patients, no change in practice should be considered based on this study.”
No funding was reported for the study. Brown reported grants from GSK funding his PhD studentship during the conduct of the study and personal fees from the World Health Organization Europe for COVID-19 surveillance consulting and from CorEvitas for unrelated consulting outside the submitted work. El-Hamamsy reports no conflicts of interest.
JAMA Cardiol. Published online August 16, 2023. Full text
Follow Marilynn Larkin on Twitter: @MarilynnL
For more from theheart.org | Medscape Cardiology, follow us on X and Facebook
Source: Read Full Article