Chronic pain-induced depression: Underlying mechanism revealed in mouse study
Chronic pain often leads to depression, which increases suffering and is clinically difficult to treat. Now, for the first time, researchers have uncovered the underlying mechanism that drives those depressive systems, according to a study published in The Journal of Clinical Investigation.
The mechanism acts to cause hypersensitivity in a part of the brain called the anterior cingulate cortex, or ACC, and knowledge of this mechanism identifies a potential therapeutic target for the treatment of chronic pain-induced depression, say Lingyong Li, Ph.D., and Kimberley Tolias, Ph.D., co-leaders of the research.
“Chronic pain is a major, unmet health issue that impacts the quality of life,” said Li, an associate professor at the University of Alabama at Birmingham Department of Anesthesiology and Perioperative Medicine. “Unfortunately, patients suffering from chronic pain have limited effective treatment options.”
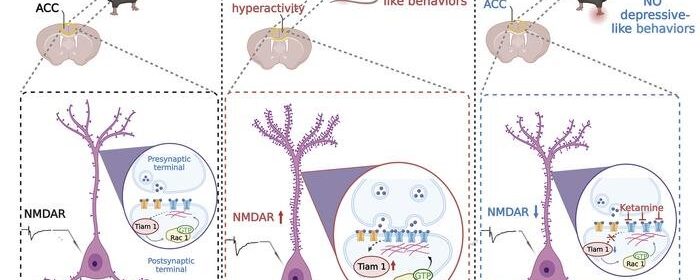
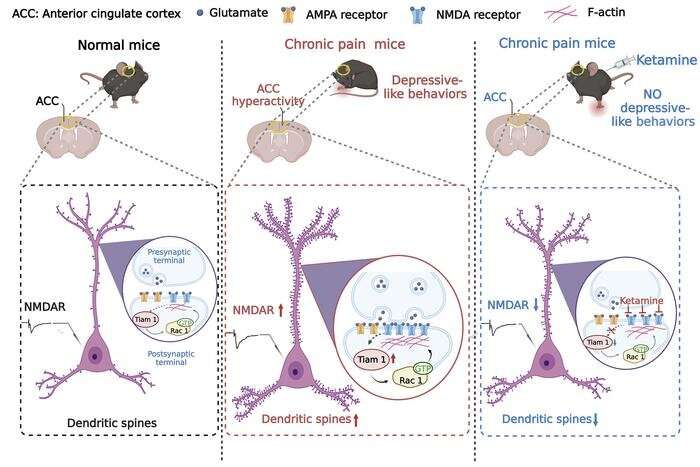
The research focused on a protein called Tiam1, which modulates the activity of other proteins that help build or unbuild the cytoskeletons of cells. Specifically, the research teams of Li and Tolias, a professor at Baylor College of Medicine, Houston, Texas, found that chronic pain in a mouse model leads to an activated Tiam1 in ACC pyramidal neurons, resulting in an increased number of spines on the neural dendrites. Dendrites are tree-like appendages attached to the body of a neuron that receive communications from other neurons.
This higher spine density increased the number of connections, and the strength of those connections, between neurons, a change known as synaptic plasticity. Those increases caused hypersensitivity and were associated with depression in the mouse model. Reversing the number and strength of connections in the model, by using an antagonist of Tiam1, relieved the mice of depression and diminished hypersensitivity of the neurons.
The ACC was already known as a critical hub for comorbid depressive symptoms in the brain. To investigate the mechanism for those symptoms, the team led by Li and Tolias first showed that Tiam1 in the ACC was activated in two mouse models of chronic pain with depressive or anxiety-like behaviors, as compared to controls.
To show that Tiam1 in the ACC modulates chronic pain-induced depressive-like behaviors, the researchers used molecular scissors to delete Tiam1 from the forebrain excitatory neurons of the mice. These mice were viable, and fertile, and displayed no gross alterations, and they still showed hypersensitivity to chronic pain. Strikingly, however, these Tiam1 conditional knockout mice did not display depressive- or anxiety-like behaviors in five different tests that gauge depression or anxiety.
When researchers specifically deleted Tiam1 from ACC neurons, they found the same results as the broader forebrain deletion. Thus, Tiam1 expressed in ACC neurons appears to specifically mediate chronic pain-induced depressive-like behaviors.
Other studies have established that an underlying cause of stress-induced depression and anxiety disorders is alterations in synaptic connections in brain regions involved in mood regulation, including the prefrontal cortex, the hippocampus and the amygdala. Li and Tolias found similar changes in dendritic neurons in the ACC for chronic pain-induced depressive-like behavior—they saw a significant increase in dendritic spine density and signs of increased cytoskeleton building. This was accompanied by increased NMDA receptor proteins and increased amplitudes of NMDA currents in the ACC neurons, both associated with hyperactivity.
These maladaptive changes were not seen in the Tiam1-knockout mice.
Researchers further showed that inhibiting Tiam1 signaling with a known inhibitor alleviated the chronic pain-induced depressive-like behaviors, without reducing the chronic pain hypersensitivity itself. The inhibition also normalized dendritic spine density, cytoskeleton building, NMDA receptor protein levels and NMDA current amplitudes.
Ketamine is a drug known to produce rapid and sustained antidepressant-like effects in chronic pain-induced depression, without decreasing sensory hypersensitivity. However, its mechanism is not fully understood. Li, Tolias and colleagues showed that ketamine’s sustained antidepressant-like effects in chronic pain are mediated, at least in part, by ketamine’s blocking the Tiam1-dependent, maladaptive synaptic plasticity in the mouse ACC neurons.
“Our work demonstrates the critical role Tiam1 plays in the pathophysiology of chronic pain-induced mood dysregulation and the sustained antidepressant-like effects of ketamine, revealing it as a potential therapeutic target for the treatment of comorbid mood disorders in chronic pain,” Li said.
Co-first authors of the study, “TIAM1-mediated synaptic plasticity underlies comorbid depression-like and ketamine antidepressant-like actions in chronic pain,” are Qin Ru and Yungang Lu, Baylor College of Medicine.
More information:
Qin Ru et al, TIAM1-mediated synaptic plasticity underlies comorbid depression–like and ketamine antidepressant–like actions in chronic pain, Journal of Clinical Investigation (2022). DOI: 10.1172/JCI158545
Journal information:
Journal of Clinical Investigation
Source: Read Full Article