Certain cancer treatment plans linked to delays

Patients undergoing primary radiotherapy treatment with or without chemotherapy, rather than surgery, for head and neck cancers are more likely to experience delays in their treatment starting, according to a new analysis from Flinders University.
The researchers say the retrospective study reflects a need to streamline referrals for cancer treatment in the healthcare system, to ensure the best possible outcome for patients.
“Head and neck cancer has the seventh highest incidence and mortality rate of all cancers worldwide and the time taken to commence treatment can have a direct result on how well the patient will respond,” says Flinders University’s Associate Professor Eng Ooi, study author and Head of Otolaryngology Head and Neck Surgery at Flinders Medical Center.
“In Australia, it is recommended that treatment be started with 56 days of the initial referral, which includes 14 days to be referred to a specialist, 14 days to be assessed by a multidisciplinary team and then 28 days from the treatment decision to the beginning of treatment.”
Cancer treatment is primarily delivered through a multi-disciplinary team approach that includes surgeons, radiation oncologists, medical oncologists and more, who discuss a patient’s case and advise a treatment plan.
“This approach generally improves treatment decision and aims to reduce the time between diagnosis and treatment, but as our analysis found, that’s not always the case,” says Associate Professor Ooi.
Looking at data from the Flinders Medical Center, the team set out to assess whether a cohort of patients newly diagnosed with head and neck cancer at the Flinders Medical Center met the recommended 56-day time frame.
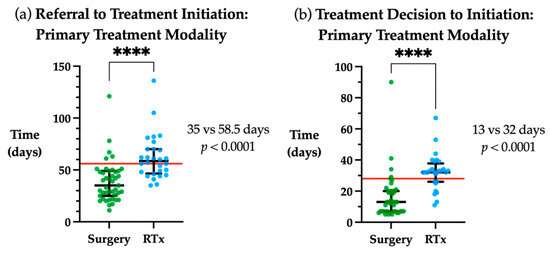
72 patients were included in the study and assessed over a 24-month period, with 28% not receiving treatment within 56 days.
When treatment plans were compared, those undergoing primary radiotherapy treatment were 8 times more at risk of not receiving treatment within the timeframe guideline, compared to those receiving a surgical intervention.
“Our analysis found the delays during any type of treatment were generally as a result of logistical challenges accessing supporting medical producers such as PET scans, dental reviews and the insertion of a gastrostomy tube, which are all often required depending on the treatment plan,” says Associate Professor Ooi.
“Given that patients undergoing primary radiotherapy are much more likely to need a PET scan, gastrostomy tube insertion and/or a pre-treatment dental review, it’s thought this is what likely leads to treatment delays.
“This is therefore the area that must be streamlined to bring about the greatest improvements, including the implementation of the resources for patients to receive prompt dental reviews, PET scans and gastrostomy tube insertion to ensure a timely start to treatment in the public healthcare system.”
While the patients who received delayed treatment did not have worse outcomes when followed up after 12 months in this particular study, the authors say the core message should still be heeded, with longer studies likely to show a negative outcome.
“There are limitations to our study, including a small sample size with limited follow-up and the potential confounding factor of delays with medical oncology, but I would expect a larger multi-center study with a longer time frame to demonstrate a significant impact to the patient when treatment is delayed,” says Associate Professor Ooi.
“It is therefore important we address the pinch points in the health care system—from diagnosis through to treatment initiation—to ensure the best possible outcome for the patients.”
Source: Read Full Article