AI now sees and hears COVID in your lungs

For Dr. Mary-Anne Hartley, a medical doctor and researcher in EPFL’s intelligent Global Health group (iGH), 2020 has been relentless. “It’s not a relaxing time to study infectious diseases,” she explained.
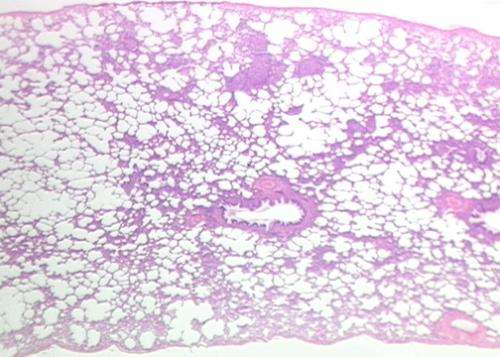
Since the beginning of the COVID-19 pandemic, Dr. Hartley’s research team has been working non-stop with nearby Swiss university hospitals on two major projects. Using artificial intelligence (AI), they have developed new algorithms that, with data from ultrasound images and auscultation (chest/lung) sounds, can accurately diagnose the novel coronavirus in patients and predict how ill they are likely to become.
iGH is based in the Machine Learning and Optimization Laboratory of Professor Martin Jaggi, a world leading hub of AI specialists, and part of EPFL’s School of Computer and Communication Sciences. “We’ve named the new deep learning algorithms DeepChest—using lung ultrasound images—and DeepBreath—using breath sounds from a digital stethoscope. This AI is helping us to better understand complex patterns in these fundamental clinical exams. So far, results are highly promising,” said Professor Jaggi.
Two university hospitals involved
CHUV, Lausanne’s University Hospital, is leading the clinical part of the DeepChest project, collecting thousands of lung ultrasound images from patients with COVID-19 compatible symptoms admitted to the Emergency Department. As principal investigator, Dr. Noémie Boillat-Blanco explains that the project started in 2019, at first trying to identify markers that would enable better identification of viral pneumonia versus bacterial ones. However, the project took a more specific COVID focus in 2020. “Many of the patients who agreed to take part in our study were scared and very ill,” she said, “but they wanted to contribute to broader medical research, just like we do. I think there is a collective motivation to learn something from this crisis and to rapidly integrate new scientific knowledge into everyday medical practice.”
At HUG, the Geneva University Hospitals, Professor Alain Gervaix, M.D., Chairman, Department of Woman, Child and Adolescent has been collecting breath sounds since 2017 to build an intelligent digital stethoscope, the “Pneumoscope.” Originally designed as a project to better diagnose pneumonia, the novel coronavirus refocused its work. The recordings have now been used to develop the DeepBreath algorithm at EPFL. Expected to be released by the end of the year it should enable the diagnosis of COVID-19 from breath sounds. Amazingly, first results suggest that DeepBreath is even able to detect asymptomatic COVID by identifying changes in lung tissue before the patient becomes aware of them.
“Pneumoscope with the DeepBreath algorithm can be compared to applications which can identify music based on a short sample played. The idea came from my daughter when I explained to her that auscultation allows me to hear sounds which help me identify asthma, bronchitis or pneumonia,” said Professor Gervaix.
Coding skills from all over the world
The algorithms have been pre-published on the EPFL website but there is still much work to do. In March, Dr. Hartley called on the EPFL community to help in a year-long hackathon called “CODED-19.” “We are continuing to refine and validate the algorithms as well as make the complex black box logic more interpretable to clinicians. We want to make robust, trustworthy tools that extend beyond this pandemic.” Work is also underway to develop an application that allows these complex deep learning algorithms to work on mobile phones, even in the most remote regions. She adds, “none of this work would have been possible without the incredible students and researchers from all over the world who have donated their time and expertise during a tumultuous period.”
Hartley, Boillat-Blanco and Gervaix are moving forward to gather more data. COVID or not, pneumonia, which kills more than one million children every year, remains one of the leading causes of death of under-fives. It’s also one of the major drivers of antibiotic resistance, affecting mostly low-income countries and communities. Says Hartley, “we want to collect data from under-represented communities so that our tools can be accurate even in poor settings. Our algorithm is for instance specifically designed to tolerate errors in image or sound collection and inconsistent quality, which are more likely in those types of settings.” They are already working on extending these models to distinguish between viral and bacterial pneumonia with the hope of drastically reducing antibiotic use.
Motivated by the potential for decentralized patient management, significant improvements in health outcomes, lowered costs and a contribution to antibiotic stewardship, Hartley has self-funded a small number of data collection probes to take to tuberculosis areas in South Africa in early 2021 and is currently trying to raise money to implement the project more broadly.
Source: Read Full Article