Role of T Cells in COVID-19

COVID-19 is an infectious respiratory disease caused by SARS-CoV-2 and the subject of an ongoing global pandemic. Infection results in an immune response leading to the production of antibodies as well as the involvement of T-cells.
.jpg)
Image Credit: GEMINI PRO STUDIO/Shutterstock.com
The vast majority of COVID-19 patients display a high number of activated T-cells that recognize the SARS-CoV-2 virus, however, some patients with severe COVID-19 have lowered T-cell counts, thus impacting on recovery.
What are T-Cells?
T-cells are a type of lymphocyte (a type of white blood immune cell) that are involved in bringing about an adaptive immune response. T-cells are so-called ‘T- ‘cells because they develop in the thymus. There are two main types of T-cells: CD8+ ‘killer’ or ‘cytotoxic’ T-cells (Tc cells), and CD4+ ‘helper’ T-cells (Th cells).
CD8+ TC cells can directly kill pathogen-infected cells as well as recruiting other immune cells by cytokine signaling to ensure a robust immune response is carried out. CD8+ TC cells express T-cell receptors (TCRs) which can recognize specific pathogenic (viral) or foreign antigens.
Any cell infected by a pathogen displays the antigen on its cell surface through class I MHC, to which specific CD8+ TC cells can bind via their TCR. This binding activates an immature CD8+ TC cell to enable it to carry out its cytotoxic (cell-killing) role.
CD4+ Th cells on the other hand can recruit B-cells (another lymphocyte which produces antibodies) amongst other cells by recognizing antigens displayed by class II MHC molecules binding to their specific TCR. Also, the cytokines released by CD4+ Th cells can allow B-cell antibody class switching as well as the activation and proliferation of CD8+ TC cells.
Image Credit: sciencepics/Shutterstock.com
Lower T-Cell Count in Severe COVID-19 Infection
COVID-19 is caused by SARS-CoV-2 infection, which originated from Wuhan, China in December 2019. The rapid spread of the novel coronavirus across the globe led to the World Health Organisation declaring it to be a global pandemic in March 2020. The symptoms of COVID-19 resemble a ‘flu’-like respiratory disease.
A high number of CD8+ TC cells are required for an effective immune response against viral infections. Some evidence (published in Frontiers in Immunology) has suggested that the number of circulating T-cell count is relatively low in some COVID-19 patients, with further reductions in those admitted to ICU, and in those over the age of 60.
The levels of circulating serum cytokines, especially TNF-α, IL-6, and IL-10 were significantly higher in patients with more severe COVID-19 (ICU admitted) compared to those with mild-moderate symptoms – however, some ICU admitted patients had ‘normal’ levels of these cytokines suggesting that these patients were immunocompromised.
The surge in cytokines in response to an infection is known as a ‘cytokine storm’ and is associated with COVID-19 related complications and hospitalization, including the development of acute respiratory distress syndrome (ARDS), and also thought to be related to the emergence of MIS-C in children and adolescents with COVID-19.
In the above study, the highest levels of TNF-α, IL-6, and IL-10 were associated with a more marked reduction in T-cell counts (both CD8+ and CD4+). Thus, this data suggests that a reduction in T-cells seen in many COVID-19 patients could be a result of high serum cytokine concentrations negatively impacting on T-cell growth. TNF-α can promote the regulated killing (apoptosis) of T-cell by interacting with TNFR1, thus the high levels of TNF-α may be directly causing a T-cell number reduction.
Another factor that can influence the rate of successful immune response is the presence of T-cell exhaustion as a result of a prolonged infection – which leads to the expression of immune-inhibition factors such as PD-1 and Tim-3.
Patients admitted to ICU/severe disease, had a higher ratio of PD-1 expressing T-cells indicative of T-cell exhaustion in severe cases of COVID-19. The levels of PD-1 & Tim-3 were very low at the prodromal stage (initial nonsymptomatic) and progressively increased during symptomatic and ICU stages.
This study highlights a potentially important mechanism by which lowered T-cell counts correlating with high serum cytokines are indicative of severe COVID-19 disease and associated with ICU admission. Furthermore, the presence of T-cell exhaustion in such patients leads to a reduced immune response where T-cells are not able to perform their functions effectively.
In such patients that display a cytokine storm, targeted therapy to combat the overactive immune response; such as by IL-6 inhibition by Tocilizumab, could be a potential way to combat the cytokine storm and allow a better recovery – although this is yet to be investigated.
High Degree of Activation of T-Cells in Most COVID-19 Cases
Whilst the above study shows weakened T-cells in some COVID-19, most other studies have shown the presence of activated T-cells in response to SARS-CoV-2 infection. In one study, it was found that almost all convalescent COVID-19 patients have CD8+ TC (70%) and CD4+ Th (100%) T cells.
Specifically, CD4+ T cells were especially responsive to the viral spike glycoprotein – which is the main target for most vaccines and therapies.
This is strong evidence that the immune system can recognize the SARS-CoV-2 virus as a threat and begin an immune response in the vast majority of cases. It is important to note that almost all COVID-19 patients develop some degree of antibodies to SARS-CoV-2 as well as T-cell activation.
The earlier study with T-cell reduction is only a hallmark of more severe cases only, and in most cases, activated T-cells help recovery by mounting an immune attack on infected cells and providing some degree of immunological memory.
In one study by Braun et al (published in medRxiv*), it was found that specifically, these TC cells are recognizing the spike glycoprotein of the SARS-CoV-2 virus – which is the main site of neutralizing antibodies against the virus. The presence of CD4+ Th cells in response to both SARS-CoV and SARS-CoV2 are generally thought to be favorable in disease outcome.
Furthermore, in this study, SARS-CoV-2 spike protein reactive CD4+ Th cells were also found in 34% of COVID-19 negative patients (compared to 83% of positive patients), suggesting a degree of similarity between other endemic “cold” coronaviruses – although these lacked specificity for the RBD for SARS-CoV-2.
Whether the presence of such T-cells that recognize elements of the spike-protein of SARS-CoV-2 in healthy subjects confers some degree of protection against COVID-19 is still to be seen. *Please note this is a preprint and has not yet been peer-reviewed.
All successful vaccines require the activation of CD4+ Th cells which stimulate B-cells to produce antibodies. The evidence suggesting a high degree of T-cell activation in response to SARS-CoV-2 infection (and to some degree in healthy non-infected individuals) is promising in that a robust immune response can be mounted either during COVID-19 infection or through preventative means. Of specific note, the recognition of the RBD is thought to be more effective in viral neutralization rather than generic viral recognition and may be the basis of longer-term immunological memory.
The problem, however, is that whilst some people may develop robust T-cells specific to the spike protein of coronaviruses including SARS-CoV-2, many individuals fail to have a robust high degree of T-cell activation to coronaviruses – such as the cold and COVID-19, and may not be protected in the long-term.
This is also evidenced by a lower than expected IgG antibody detection in some recovered patients. Thus, understanding what elicits a robust immune response – likely the recognition of the RBD of SARS-CoV-2 – is important if vaccines are to be successful in providing longer-term immunity.
Why some patients develop severe immune reactions to SARS-CoV-2 infection including an exhausted phenotype in addition to T-cell reduction is still not fully understood, though it is thought age, sex, genetics, and lifestyle can influence this. Conversely, why some healthy individuals develop CD4+ Th cells protective of SARS-CoV-2 through recognizing similar spikes of endemic coronaviruses is also an interesting and potentially important research question.
In summary, a vast majority of COVID-19 patients develop an immune response against SARS-CoV-2 with the activation of T-cells to the spike-protein of the virus. By recognizing the spike-protein specifically the receptor-binding domain – which is the most effective site for neutralizing antibodies – a robust immune response can be mounted and may remain protective for future infections.
In a minority of patients that develop more severe disease, reduced T-cell count with an ‘exhaustive’ phenotype may be associated with a ‘cytokine storm’, impacting recovery.
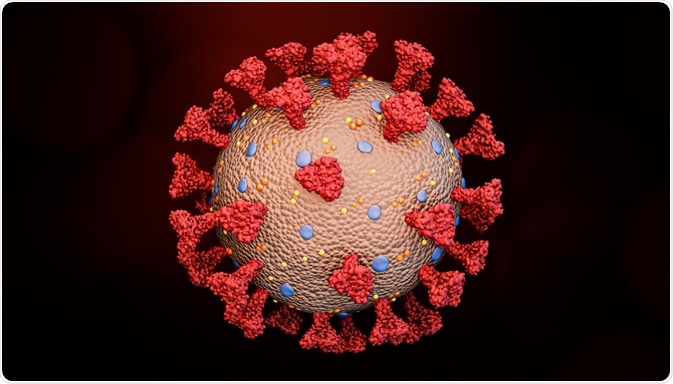
Image Credit: MattLphotography/Shutterstock.com
Sources:
- Diao et al, 2020. Reduction and Functional Exhaustion of T Cells in Patients With Coronavirus Disease 2019 (COVID-19). Front Immunol. 11: 827. https://pubmed.ncbi.nlm.nih.gov/32425950/
- Braun et al, 2020. Presence of SARS-CoV-2 reactive T cells in COVID-19 patients and healthy donors. medRxiv (preprint server) https://doi.org/10.1101/2020.04.17.20061440 *please note that this is a preprint and not yet peer-reviewed or published in a scientific or medical journal
- Grifoni et al, 2020. Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell. 181(7): 1489–1501.e15. https://pubmed.ncbi.nlm.nih.gov/32473127/
- Weiskopf et al, 2020. Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci Immunol. 5(48):eabd2071 https://pubmed.ncbi.nlm.nih.gov/32591408/
Further Reading
- All Coronavirus Disease COVID-19 Content
- What Mutations of SARS-CoV-2 are Causing Concern?
- What is the Clinical Impact of COVID-19 on Cancer Patients?
- Can Pets Get COVID-19?
- An Overview of the SARS-CoV-2 Vaccines
Last Updated: Jul 6, 2020

Written by
Osman Shabir
Osman is a Neuroscience PhD Research Student at the University of Sheffield studying the impact of cardiovascular disease and Alzheimer's disease on neurovascular coupling using pre-clinical models and neuroimaging techniques.
Source: Read Full Article