Differences in the Brains of People with Severe Mental Illnesses

According to a recent study, persons with severe mental illness do not necessarily share similar brain activities in response to certain social tasks.
Rather, those with and without mental illness tend to have one of three responses that do not relate to whether or not they have been diagnosed with a mental illness.
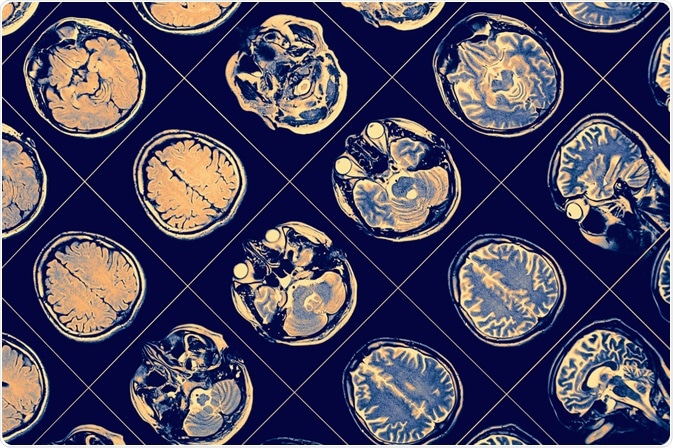
Image Credit: sfam_photo/Shutterstock.com
How does mental illnesses change brain activity?
Severe mental illnesses, such as schizophrenia, cause both structural and functional alterations in the brain, which may be noted on imaging studies, but are also generally insufficient to diagnose mental illness.
In the case of chronic brain disorders such as schizophrenia, enlargement of brain ventricles (brain cavities that contain cerebral spinal fluid) occurs as a result of brain tissue atrophy. Another most common alteration is the reduction of gray matter in the brain due to cell compression. This change is more prominent in the frontal and temporal lobes.
Such changes in the size of different brain parts cause alteration in the brain’s communicating network, leading to functional abnormalities.
In terms of symptoms, a schizophrenic patient is known to have impaired social behavior, in addition to having a lack of concentration, delusion, hallucination, thinking difficulties, and reduced level of motivation.
All these common signs and symptoms, as well as the typical structural and functional features of the brain, form the predictable diagnostic categories, which are being utilized by the doctors to diagnose the mental condition.
Is there any difference in brain activity among patients with severe mental illness?
According to scientific literature, people with severe mental disorders do not share similar brain characteristics, and some of them have brain activities similar to their healthy counterparts. This finding supports the evidence that there is heterogeneity in severe mental health conditions.
In this context, multi-site research involving 109 people with schizophrenia spectrum disorder has found that schizophrenic patients can be sub-grouped into three categories with distinct patterns of brain activities. These sub-groups can be defined as ‘typical’, ‘hyperactivated’, and ‘deactivated’ profiles.
Upon comparing the results of socio-emotional and neurocognitive tests with corresponding brain activities, it can be said that people with hyperactivated brain profiles possess deprived brain activities, and they need more mental power to complete a behavioral task compared to their peers.
In contrast, people with deactivated brain profiles are likely to have an efficient neural network and brain activities and need to put much less effort to perform a task compared to the other groups. These findings provide clear-cut evidence on differential brain activity patterns among both persons with severe mental illness and healthy persons.
Why it is important to define sub-groups?
People with severe mental illnesses like schizophrenia are known to have social behavioral impairments that can lead to social isolation, functional disabilities, depression, anxiety, and reduced overall quality of life.
Since there is no actual treatment to enhance one’s social behavioral skills, it is important to identify specific brain activities related to social responses that can be targeted to make effective treatment strategies. This can open up a new path toward personalized medicine.
In the case of identifying new therapeutic interventions for mental illnesses, it is important to focus more on alterations in the brain networking system instead of dealing with symptoms alone.
Unfortunately, most of the therapeutic research mainly aims at comparing a disease group with a healthy control group, which can typically provide only subtle information.
The identification of sub-groups among people with schizophrenia can break the conventional pattern of therapeutic research design, as it is now evident that the association between a person’s brain activity and social response is not at all related to conventional diagnostic categories.
Sources
- Hawco C. 2019. Separable and Replicable Neural Strategies During Social Brain Function in People With and Without Severe Mental Illness. The American journal of psychiatry. https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2018.17091020
- Science Daily. 2019. Brains of people with schizophrenia-related disorders aren't all the same https://www.sciencedaily.com/releases/2019/01/190104121423.htm
- The US. News. 2019. Inside the schizophrenic brain. health.usnews.com/…/inside-the-schizophrenic-brain
Further Reading
- All Mental Health Content
- World mental health support and the effect of stigma and discrimination
- Pollution and Mental Health
- Mental Health Nursing
- Treatment Options for Intrusive Thoughts
Last Updated: Mar 30, 2020

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article