Congenital vs Acquired Facial Palsy

Facial palsy or paralysis arises as a result of injury to the seventh cranial nerve, which is called the facial nerve. This nerve has its origins in the pons and winds its way through the skull, before exiting through the stylomastoid foramen on the temporal bone.
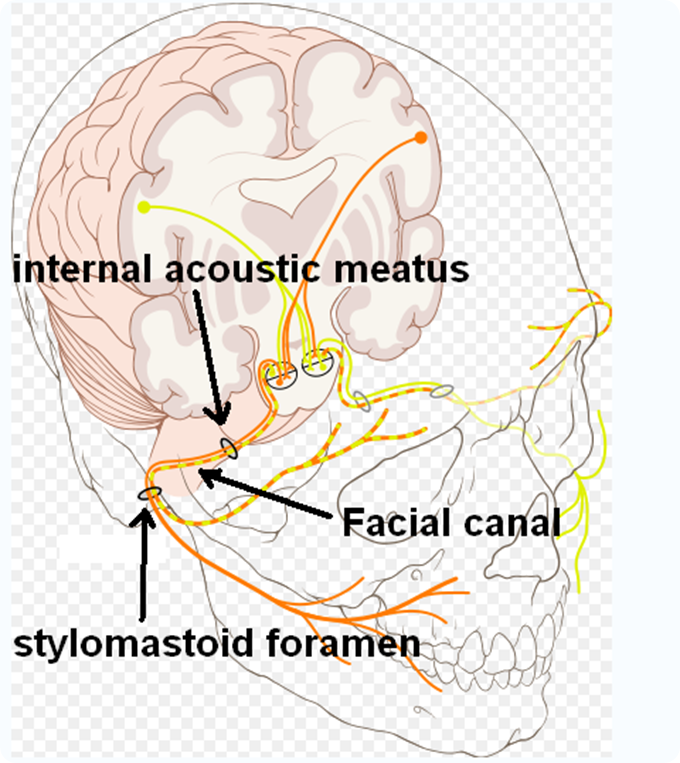
Cranial nerve VII 7, with facial canal Highlighting. Credits: Patrick J. Lynch, medical illustrator; C. Carl Jaffe, MD, a cardiologist. https://creativecommons.org/licenses/by/2.5/ / id.wikipedia.org.
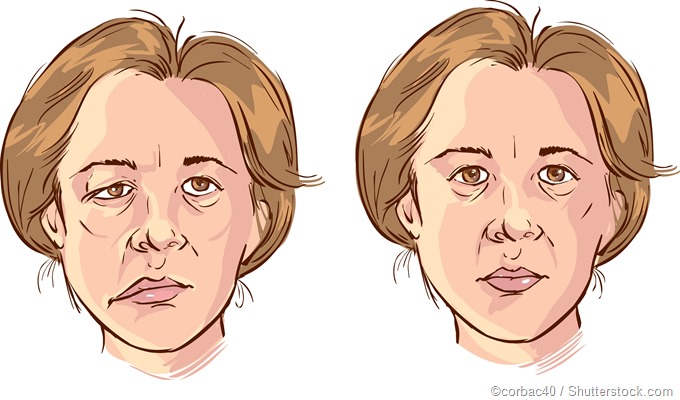
Injury to this nerve results in loss of control of the facial muscles, with consequent drooping of the face. It may be uni- or bilateral. This loss of control of the facial muscles may be temporary or permanent, depending on the etiology, and may affect the eyes, mouth and other areas of the face.
Congenital facial paralysis
Children who present with facial palsy at birth are said to have congenital facial paralysis (CFP), which is rare. It tends to be associated with other facial and bodily dysmorphologies, including cleft palate and deformed extremities. CFP may be classified as uni- or bilateral; developmental or traumatic; and complete or incomplete. CFP is responsible for up to 14% of cases of facial paralysis in the pediatric population.
Etiology
The majority of cases arise due to a traumatic episode during childhood, and of these traumatic cases about 90% are associated with forceps delivery.
Teratogens and syndromes are implicated in the developmental causes of CFP. Mobius syndrome is one such example. It involves the congenital absence of the sixth and seventh cranial nerves. These children are unable to control eye movement or produce facial expressions. They cannot frown, blink, smile, move their eyes to the side, or suck properly. Congenital unilateral lower lip palsy is another and more common developmental disorder that results in facial asymmetry visible when the affected baby is crying.
Thalidomide, which is a sedative and antiemetic drug, and misoprostol, which is a synthetic prostaglandin, are teratogens known to be associated with CFP. Thalidomide causes phocomelia (i.e. underdeveloped or absent limbs), in addition to failure of development of the ear, and of the abducent and facial nerves. Thalidomide, which is used for conditions such as leprosy and multiple myeloma, should be avoided in pregnancy. Misoprostol, based on studies, has been linked to Mobius syndrome, which is believed to be due to a disruption in the vasculature of the subclavian artery in the 4th to 6th week of gestation.
Management
Managing CFP may involve both pharmacotherapy and surgery where applicable. Babies require the use of artificial tears during their waking hours, and eye ointments during sleep, to prevent eye dryness because of inability to close the eyelids completely. Children who have CFP of traumatic etiology are recommended to receive observation and corticosteroid treatment for a set period before decompression of the nerve and other surgical techniques are attempted. This is because 90% or more of all traumatic CFP cases resolve spontaneously over time.
Surgery is warranted in infants who fail to show significant improvement after 5 weeks or if there is an absence of evoked responses to muscles innervated by the facial nerve after the 5th day of life. Other indications for surgery include displaced temporal bone fractures, complete unilateral paralysis at birth, and the presence of blood in the middle ear or tympanic cavity. Surgical options include decompression, neurorrhaphy, cable grafts, nerve transposition, and muscle transfers, among others.
Acquired facial paralysis
In contrast to CFP, acquired facial paralysis (AFP) is not present at birth and may appear at any time during life.
Etiology
Common causes of AFP include infection, inflammation, stroke, tumors, iatrogenic injury and trauma. Facial palsy may also be acquired after infections with herpes simplex virus (HSV) and Lyme disease. However, in nearly 60% of cases, AFP is idiopathic, although it is believed that this too is a delayed result of infection with HSV. Idiopathic AFP is referred to as Bell’s Palsy (BP).
The symptoms of BP tend to develop rather quickly and reach peak intensity at around 48 hours. Patients may experience paralysis on one side of the face and have difficulty closing their eyes, increased dryness, or excessive tears. There may be difficulties with speaking, eating, or drinking, and some patients may experience headaches, dry mouth, dizziness and drooling. Tumors anywhere along the path of the facial nerve may also cause the symptoms of facial nerve paralysis. However, these do not have an acute onset as in the case of BP.
Inadvertent injury to the facial nerve may occur during the removal of tumors, resulting in facial paralysis. The most common surgery implicated is the removal of acoustic neuromas. In addition to cerebrovascular incidents, other causes of AFP, although rare, include otitis media, neurosarcoidosis and multiple sclerosis. Treatment of AFP depends on the etiology, but may include pharmacotherapy with corticosteroids and antiviral agents for infectious causes, or surgical operations for tumors and trauma. Physiotherapy may also be necessary for some patients.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677084/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671829/
- http://www.nhs.uk/Conditions/Bells-palsy/Pages/Introduction.aspx
- http://jamanetwork.com/journals/jama/fullarticle/184482
- http://www.cmft.nhs.uk/royal-eye/our-services/facial-function-clinic.aspx
Further Reading
- All Facial Palsy Content
- What is Facial Palsy?
- Facial Nerve Decompression
- Bell’s Palsy Pathology
- What is Bell’s Palsy?
Last Updated: Feb 26, 2019

Written by
Dr. Damien Jonas Wilson
Dr. Damien Jonas Wilson is a medical doctor from St. Martin in the Carribean. He was awarded his Medical Degree (MD) from the University of Zagreb Teaching Hospital. His training in general medicine and surgery compliments his degree in biomolecular engineering (BASc.Eng.) from Utrecht, the Netherlands. During this degree, he completed a dissertation in the field of oncology at the Harvard Medical School/ Massachusetts General Hospital. Dr. Wilson currently works in the UK as a medical practitioner.
Source: Read Full Article