Bowel Preparation for Colectomy: Risks to Watch For

A colectomy is a procedure that involves removing all or a portion of the colon. Although it's commonly recommended as an intervention for patients with colon cancer, it is also an option for some patients that have other ailments.
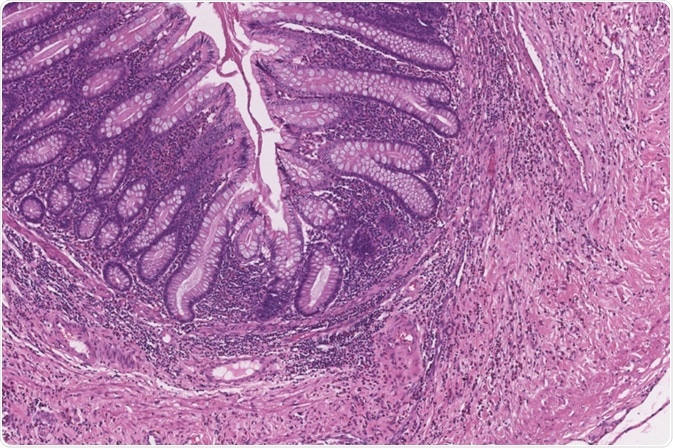
Image Credit: Java Jar/Shutterstock.com
For example, if a patient has ulcerative colitis or Crohn's disease that is not well controlled with medication, or if a colonoscopy shows precancerous lesions, a doctor may recommend a total or partial colectomy. A colectomy can also be a treatment option for patients with bowel obstructions.
Concerning cancer, specifically, a surgeon may only remove small segments of a cancer patient's colon at first, and potentially extract more as the patient's illness progresses. Moreover, if a person has an exceptionally high risk of developing cancer due to the presence of numerous precancerous colon polyps, a physician may recommend a colectomy as a preventative measure.
Colectomy patients usually go through bowel preparation measures before the procedure. Taking these steps can reduce the risks a person faces.
Reducing surgical site infections with a combined approach
Surgical site infections (SSI) are risks that can manifest after a person undergoes a colectomy. Two of the main ways to reduce such complications are to put the patients on a regimen of oral antibiotics and to prescribe mechanical bowel preparation, whereby a person ingests a liquid that stimulates the clearing of the bowel.
The removal of feces from the body reduces the bacteria that could contribute to future infections. There is a debate in the medical community about whether patients should receive oral antibiotics, instructions for mechanical bowel preparation or do both of those things to reduce the risks of colectomy complications.
A 2018 meta-analysis examined the results of 38 randomized clinical trials with a total patient pool of 8,458 patients who were undergoing elective colectomies. The goal was to see which preparation methods proved most effective for reducing SSI.
One group only took oral antibiotics, while another solely did mechanical bowel preparation. A third group received both preparatory measures, and a fourth had no bowel preparation at all.
The results showed that patients who underwent mechanical bowel preparation and received oral antibiotics had the lowest rate of organ/space and incisional infections. An anastomotic leak, whereby the luminal contents start to seep from two parts joined during surgery, is another risk associated with colectomy.
However, this research did not show substantial reductions in that complication for any single bowel preparation method — or lack thereof — versus another.
Thus, if physicians are trying to decide between instructing a patient to follow a schedule for mechanical bowel preparation or prescribe them a round of oral antibiotics, the ideal approach may be to do both.
Specific Infections May Persist After a Colectomy
Clostridium difficile, sometimes called C. diff, is a type of spore-forming bacteria that lives in the bowel. C. diff infections can cause life-threatening complications, including colon inflammation. Research published in 2009 showed isolated cases whereby C. difficile enteritis affects the small bowel and requires treatment with antibiotics.
However, a more recent case concerned an allogeneic stem cell recipient who developed a recurrent C. difficile infection after a total colectomy. The researchers clarified that the patient is the only person in that situation to develop such an infection. Although this case was the first involving a stem cell patient, there are other reported cases of C. diff infections in colectomy patients.
Thus, physicians must be aware of and tell patients about the risks associated with colectomies and these kinds of infections. Such information should be given throughout a patient's care. Regarding colon cancer, a person may need further treatments after a full or partial colectomy, depending on whether cancer spreads. This is due to the risk of additional health issues such as colorectal liver metastasis, which may require another surgery.
It occurs when cancer spreads to the liver from the colon or rectum. Doctors tend to discover this issue during routine screenings as well as appointments that occur after a colon removal procedure. Physicians can help people understand the risks of C. diff infections as well as other complications and associated procedures during their conversations about colectomy risks.
Finnish study indicates bowel preparation may not help
Many physicians view bowel preparation as an essential step to help colectomy patients reduce the risk of things going wrong associated with the procedure. However, a 2019 study suggests the need to revisit whether it's effective in cutting down the probability of complications.
Patients at four hospitals in Finland who were undergoing colectomies got randomly assigned to either undergo mechanical bowel preparation and take oral antibiotics or not participate in those measures at all.
The results associated with these 400 patients showed that bowel preparation did not reduce the rate of SSI or morbidity in the patients. Moreover, there was no difference in the groups regarding the length of the required hospital stay.
The researchers suggest further investigations into the efficacy of bowel preparation before colectomies. The team pointed out that bowel preparation is stressful for patients, but the study’s conclusions indicate it does not benefit them.
Considerations for future conversations with colectomy candidates
The research covered here may reshape physicians' decisions as they determine whether or not to have colectomy patients go through with bowel preparation measures and, if so, which options to use.
However, a health care provider must always engage in thorough discussions with the people in their care and take all personal and case-related factors into account when assessing the best ways to minimize risks.
Sources:
- Toh J, Phan K, Hitos K, et al. Association of mechanical bowel preparation and oral antibiotics before elective colorectal surgery with surgical site infection. JAMA Network Open. 2018;1(6):e183226. doi:10.1001/jamanetworkopen.2018.3226
- Causey MW e. Clostridium difficile enteritis after colectomy. – PubMed – NCBI. Ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/pubmed/19999913. Published 2009. Accessed February 3, 2020.
- Chang K, Kreuziger L, Angell K, Young J, Ustun C. Recurrence of Clostridium difficile infection after total colectomy in an allogeneic stem cell transplant patient. Bone Marrow Transplant. 2011;47(4):610-611. doi:10.1038/bmt.2011.132
- Fraiman M. Liver Surgery for Colorectal Metastasis to the Liver. Baltimore Liver & Pancreas Surgeon – Dr. Mark Fraiman. liverandpancreassurgeon.com/…/. Published 2018. Accessed February 3, 2020.
- Koskenvuo L, Lehtonen T, Koskensalo S et al. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (MOBILE): A multicentre, randomised, parallel, single-blinded trial. The Lancet. 2019;394(10201):840-848. doi:10.1016/s0140-6736(19)31269-3
- Lehtinen P. A Finnish study finds bowel preparation for colon surgery unnecessary | University of Helsinki. University of Helsinki. www.helsinki.fi/…/a-finnish-study-finds-bowel-preparation-for-colon-surgery-unnecessary. Published 2019. Accessed February 3, 2020.
Further Reading
- All Colon Cancer Content
- What Causes Colorectal Cancer?
- What is Colorectal Cancer
- Colorectal Cancer Diagnosis
- Colorectal Cancer Prevention
Last Updated: Apr 14, 2020

Written by
Kayla Matthews
Kayla Matthews is a MedTech journalist and writer. Her interest in medical technologies grew out of her larger interest in medical technology, science, and gadgets.Previously, Kayla has been a senior writer for the popular technology site MakeUseOf, as well as had her writing featured on well-known sites such as The Week, The Observer, Computerworld, and The Daily Dot.In the medical and healthcare space, Kayla’s work has been featured on a number of prominent websites. These include SpringerOpen, HIT Consultant, HealthIT Outcomes, Medical Economics and Healthcare Innovation.
Source: Read Full Article