Blood Type Testing

A blood type is classified by the presence or absence of antibodies and certain antigens on the surface of the red blood cells (RBCs). There are four distinct blood types; A, B, AB and O. Transfusion with the wrong blood type can lead to life-threatening consequences, and therefore, tests to determine the blood type is extremely important before a blood transfusion.

ABO Blood Groups
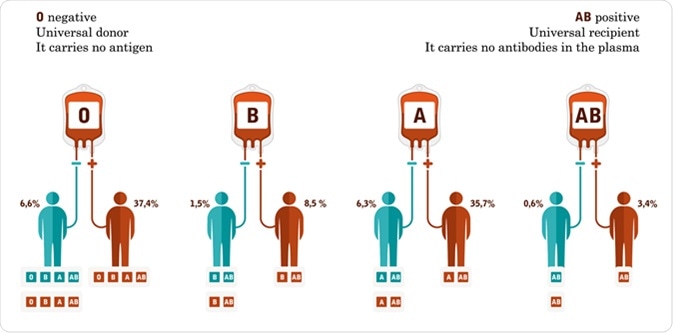
The four ABO blood groups are determined by antigens that are present on the surface of the RBCs. Type A individuals have type A antigens, type B individuals have type B antigens, type AB individuals have both type A and B antigens, and type O individuals have no antigens. In addition, all individuals have antibodies within their serum. Therefore, type A blood serum contains type B antibodies, type B blood serum contains type A antibodies, type AB blood serum contains no antibodies, and type O blood serum contains both A and B antibodies.
If an individual with type B blood is transfused with type A blood, the type A antibodies within their serum will detect and bind to the antigens of the type A blood cells, leading to agglutination. This can lead to severe, life-threatening blood clots. Type O individuals can therefore only receive type O blood as their serum contains both types of antibodies. However, these individuals are considered “universal donors” as their serum contains no antigens and therefore antibodies present in a recipient’s serum cannot agglutinate during transfusion with Type O blood.
Rhesus Blood Groups
Each blood type also has two different classifications, positive and negative. This identifies if the individual has the Rhesus factor (Rh) antigens within their blood. If an individual has these antigens, then they are Rh positive, whereas if they do not, they are Rh negative.
The Rh factor also influences the type of blood that an individual can receive. An individual, who is Rh positive, can accept both positive and negative blood. However, individuals who are Rh negative can only accept blood from other negative donors. This is because the presence of the antibodies in the blood of Rh-positive donors will lead to agglutination.
How to Determine the Blood Group
Determination of the blood type is crucial in various situations such as before blood donation or transfusion, organ transplant, or during pregnancy.
There are two stages to determine the blood group, known as ABO typing. The first stage is called forward typing. In this method, RBCs are mixed with two separate solutions of type A or type B antibodies to see if they agglutinate. If this blood clumps, this indicates the presence of antigens within the blood sample. For example, a sample of type A blood will clump when tested with type B antibodies as it contains type A antigens. Whereas, a type O blood sample will not agglutinate with either type A or type B antibodies as type O blood contains no antigens.
To ensure the accuracy of this process, a secondary stage called reverse typing is used. In this method, plasma is combined with separate solutions of type A or type B blood. Clumping can therefore be monitored to confirm the results obtained during the forward typing process.
Rh typing is similar to ABO typing. First, a blood sample is mixed with RhD antibodies. Clumping again suggests the presence of antigens, and so indicates that an individual is Rh positive.
Pregnancy
Blood tests in pregnant women are vital, particularly if a mother is RhD negative, and the unborn child is RhD positive. RBCs from the baby can be passed into the mother’s blood via the placenta and lead to production of antibodies against Rh antigens. However, these antibodies do not cause any harm in the first-born. In subsequent pregnancies with an RhD positive baby, these antibodies can attack the babies’ blood cells leading to severe anemia in the child. This condition is called the Hemolytic disease of the newborn. This condition can be fatal if left untreated. This can also occur in case of mismatches with ABO blood types; however, these cases are often not as severe.
Future of ABO Typing
Numerous strategies are emerging in the area of blood group typing. Blood group genotyping is one field that is being used extensively to determine the nature of the blood group antigens in patients with autoimmune disorders or in patients that require transfusion therapy or chemotherapy. This is because blood group genotyping provides detailed information on the nature of the blood group antigens on the surface of the erythrocyte. This can rule out any ambiguity that is usually associated with serological methods.
Although the traditional method of blood group typing is still considered as the most reliable method, focused and sustained research should be continued in this field to develop synthetic antibodies that are capable of selective recognition of different ABO groups. This will help ABO blood typing mature into a robust scientific technology.
Sources
- https://www.nhs.uk/conditions/blood-groups/
- http://www.whatsmybloodtype.org/types.html
- https://medlineplus.gov/ency/article/001298.htm
- https://patient.info/doctor/blood-transfusion-reactions
- http://www.mydr.com.au/tests-investigations/blood-typing
- www.blood.co.uk/…/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4732084/
Further Reading
- All Blood Test Content
- NIPT Test (Noninvasive Prenatal Testing)
- Understanding Laboratory Blood Test Results
- Do We Need Transgender-specific Reference Ranges for Common Laboratory Tests?
Last Updated: Feb 26, 2019

Written by
Hannah Simmons
Hannah is a medical and life sciences writer with a Master of Science (M.Sc.) degree from Lancaster University, UK. Before becoming a writer, Hannah's research focussed on the discovery of biomarkers for Alzheimer's and Parkinson's disease. She also worked to further elucidate the biological pathways involved in these diseases. Outside of her work, Hannah enjoys swimming, taking her dog for a walk and travelling the world.
Source: Read Full Article