take clomid even if ovulate

In a recent study published in the journal Morbidity and Mortality Weekly Report, researchers analyzed the United States (US) Centers for Disease Control and Prevention's (CDC's) National Notifiable Disease Surveillance System (NNDSS) data on congenital syphilis cases across the country. Their findings revealed that lack of testing and appropriate treatment were responsible for almost 90% of congenital syphilis in 2022, resulting in 231 stillbirths and 51 infant deaths. Comparisons with reports from 2021 reveal a 31.7% increase in the number of patients in just one year. Improved prenatal care, timely diagnosis, viagra bestellen express and effective clinical interventions could help prevent the disease and reverse this alarming trend.
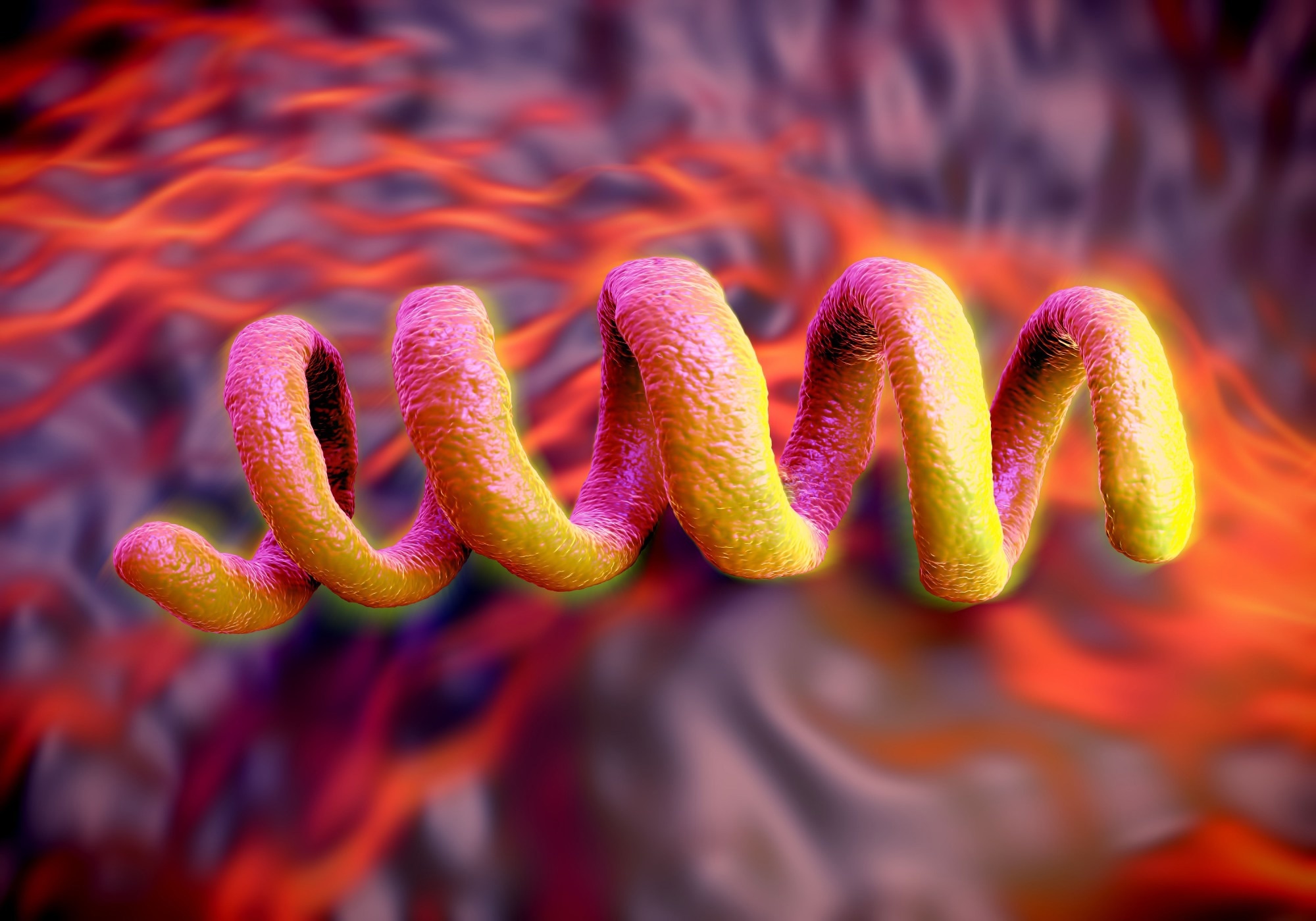 Study: Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. Image Credit: Peddalanka Ramesh Babu / Shutterstock
Study: Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. Image Credit: Peddalanka Ramesh Babu / Shutterstock
Congenital syphilis and its associated risks
Syphilis is a sexually transmitted disease (STD) caused by the syphilis bacteria Treponema pallidum. It is usually painless, with symptoms including sores on the genitals, rectum, and mouth. Based on the progression of the disease, syphilis infections are categorized into four main stages – primary, secondary, latent, and tertiary. With adequate medication, usually antibiotics, syphilis is a curable condition, though the damage caused during disease progression may result in permanent scars.
Congenital syphilis involves the transmission of syphilis from an infected mother to her child during pregnancy or childbirth. Given the underdeveloped immune systems of embryos and newborns, the effects of syphilis are significantly more severe than in adults, often resulting in stillbirths, miscarriages, or infant mortality during the first few days of life. Even for infants that survive the infection, the risk of lifelong blindness, loss of hearing, stunted development, and skeletal abnormalities is high.
Alarmingly, while other STDs, including the human immunodeficiency virus (HIV) and hepatitis B, are on the decline in the United States (US), the years 2012 through 2021 saw a 755% increase in reported congenital syphilis. This trend depicts a strong association with syphilis infections in women, which rose by 676% in the same time period. Observational reports suggest a geographical and ethnic disparity in syphilis prevalence, which might explain the concerning increase in congenital syphilis despite the CDC's recommendations for syphilis screening during the first prenatal care visit.
"CDC recommends screening at 28 weeks' gestation and at delivery for those who 1) live in communities with high rates of syphilis, 2) are at high risk for syphilis acquisition during pregnancy (e.g., substance use or a new sex partner), or 3) were not previously tested during the pregnancy."
Validating and recognizing observed disease prevalence disparity and taking measures to curb missed opportunities (lack of- or delayed diagnosis and treatment) is essential in reducing mortality and morbidity due to this curable condition.
About the study
This study's data was obtained from the CDC's National Notifiable Diseases Surveillance System (NNDSS) and comprised congenital syphilis records from all 50 US states, territories, and the District of Columbia. Congenital syphilis occurrences were classified into one of six categories based on potential missed prevention opportunities. These included: 1. No documented testing/untimely testing, 2. No treatment or undocumented treatment, 3. Late identification, 4. Inadequate treatment, 5. Congenital syphilis, despite adequate testing and treatment, and 6. Data deficit.
Timely testing was defined as testing more than 30 days before delivery. The study cohort comprised all women between the ages of 15 and 44, and demographic and geographical data was obtained from the US Census Bureau.
Study findings
CDC NNDSS data revealed a total of 3,761 cases of congenital syphilis in 2022. Of these, 231 (6%) resulted in stillbirths and 51 (1%) neonatal deaths. These findings equate to a 31.7% increase in congenital syphilis cases compared to 2021. This corresponds to a 17.2% increase in syphilis cases among women between the ages of 15 and 44 and a 10-fold increase over the previous 10 years.
Statistical analyses revealed that a lack or untimely testing was responsible for 36.8% of all congenital syphilis cases (N = 1.385), undocumented or no treatment in 11.2% (N = 423), and inadequate treatment in 39.7% (N = 1,494). One hundred and nine-seven (5.2%) cases were diagnosed later than 30 days before delivery. Surprisingly, despite clinically documented adequate treatment, 130 newborns were reported to have syphilis (3.5%).
Disparity analyses revealed that the West, Northeast, and Midwest regions showed the highest concentrations of no- or untimely testing (56.2%, 50.0%, and 40.4%). Alarmingly, the Midwest comprised the greatest region concentration of female syphilis cases for 2022. White Americans (40.8%) depicted much lower congenital syphilis prevalence compared to non-Hispanic American Indians or Alaska Natives (47.4%) and Pacific Islanders (61.0%). Inadequate treatment despite accurate and on-time diagnoses was most prevalent in Black (39.2%) and Latino (47.4%) cases.
Conclusions
The present study investigates the factors responsible for the increasing rate of congenital syphilis cases in America. Their findings suggest that the growing number of syphilis cases in American women between the ages of 15 and 44, combined with a lack of timely testing and/or adequate treatment, are the underlying factors behind these observations.
"Congenital syphilis rates are rapidly increasing in the United States and are at the highest level in at least 30 years. Barriers to congenital syphilis prevention are multifactorial, including those at the patient level, such as substance use and insurance status, and those at the system level, such as structural inequities, limited access to health care, and medication shortages. Addressing patient and system-level barriers to accessing testing, treatment, and care could help prevent congenital syphilis. Improvements in timely testing and appropriate treatment of syphilis through tailored strategies at local and national levels will help control the congenital syphilis epidemic in the United States."
- McDonald R, O'Callaghan K, Torrone E, et al. Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. MMWR Morb Mortal Wkly Rep. ePub: 7 November 2023, DOI: http://dx.doi.org/10.15585/mmwr.mm7246e1, https://www.cdc.gov/mmwr/volumes/72/wr/mm7246e1.htm
Posted in: Child Health News | Medical Research News | Women's Health News
Tags: Bacteria, Blindness, Childbirth, Congenital Syphilis, Health Care, Hearing, Hepatitis, Hepatitis B, HIV, Immunodeficiency, Mortality, Pregnancy, Prenatal, Syphilis, Virus

Written by
Hugo Francisco de Souza
Hugo Francisco de Souza is a scientific writer based in Bangalore, Karnataka, India. His academic passions lie in biogeography, evolutionary biology, and herpetology. He is currently pursuing his Ph.D. from the Centre for Ecological Sciences, Indian Institute of Science, where he studies the origins, dispersal, and speciation of wetland-associated snakes. Hugo has received, amongst others, the DST-INSPIRE fellowship for his doctoral research and the Gold Medal from Pondicherry University for academic excellence during his Masters. His research has been published in high-impact peer-reviewed journals, including PLOS Neglected Tropical Diseases and Systematic Biology. When not working or writing, Hugo can be found consuming copious amounts of anime and manga, composing and making music with his bass guitar, shredding trails on his MTB, playing video games (he prefers the term ‘gaming’), or tinkering with all things tech.