songs for lyrical solo
Investigators from Cedars-Sinai Cancer, working in collaboration with colleagues in Colorado and the Netherlands, have identified a specific type of bladder cancer most likely to resist first-line treatment. Their study, published today in Science Translational Medicine, could guide clinicians toward more aggressive treatment or more targeted therapies for some patients with specific subtypes of the disease, ultimately saving lives.
“These findings provide a potential tool for determining how well patients initially treated for high-risk bladder cancer that isn’t yet muscle-invasive will respond to the most common follow-up therapy, curso de funilaria e pintura automotiva em campinas ” said Dan Theodorescu, MD, Ph.D., co-senior author of the study and director of Cedars-Sinai Cancer and the PHASE ONE Distinguished Chair. “With this information, clinicians can make more informed and timely decisions about aggressive surgical treatment or take advantage of new options being created through precision medicine.”
More than 80,000 Americans are diagnosed with bladder cancer each year, and the majority of their tumors are non-muscle invasive, meaning they are found in the tissue that lines the inner surface of the bladder and do not involve the bladder muscle. These tumors are classified as low-, intermediate- or high-risk based on their size, speed of growth and how likely they are to spread.
Once a tumor has been surgically removed, most patients with higher-risk tumors receive a course of immunotherapy called Bacillus Calmette-Guérin (BCG). BCG therapy is designed to help the body’s immune system fight off cancer recurrence, but it benefits only 50% of patients with high-risk non-muscle invasive bladder cancer.
For the remaining 50%, the cancer comes back within five years, and these patients have a 20% risk of progressing to advanced disease and high mortality rates.
“Patients who don’t respond have been exposed to unnecessary toxicity from BCG treatment, and because of the delay in receiving more aggressive treatment, their chances of survival may have been compromised,” Theodorescu said. “Our goal with this study was to find a new way to identify these patients before they receive BCG therapy and direct them immediately to surgical removal of the bladder or other more aggressive therapies, which may reduce quality of life but have excellent long-term outcomes.”
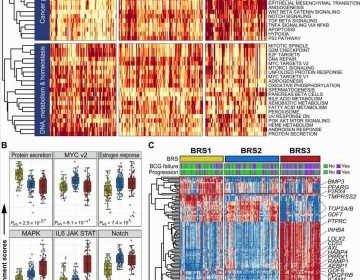
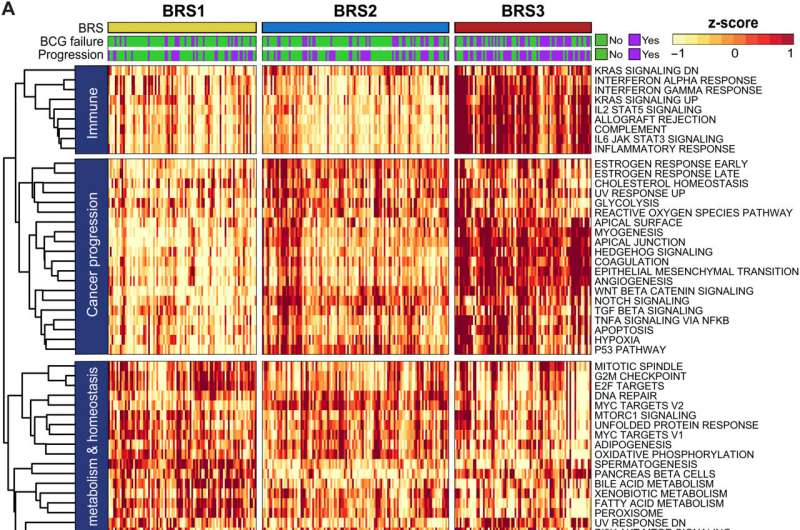
To do so, investigators used molecular profiling of non-muscle invasive bladder cancers from 132 patients who had never received BCG treatment, and 44 patients whose cancer recurred following BCG treatment. They identified three distinct subtypes among these tumors and matched them with patients’ clinical outcomes to determine whether the subtypes were linked with cancer recurrence.
One of the subtypes, which investigators call BCG Response Subtype 3 (BRS3), was more closely associated with reduced progression-free survival—meaning less time until the cancer recurred—than the other two subtypes. And the study findings showed that BRS3 was the dominant subtype among patients whose cancer recurred after BCG therapy.
The investigators were also able to show that a commercially available test can accurately identify BRS3 tumors. A larger follow-up study is underway to further validate this finding.
Theodorescu received a presidential citation from the American Urological Association for “elucidating the underpinnings of urothelial cancer,” which is the most common type of bladder cancer, at the 2023 AUA Annual Meeting in April.
“I’m very humbled and honored to be recognized by clinical peers at the American Urological Association,” Theodorescu said. “This citation recognizing my scientific achievements means a lot to me.”
Theodorescu first took an interest in bladder cancer as a graduate student in the 1990s, has worked in the field ever since, and has continued building an international network of collaborators.
“What is particularly satisfying about this study is that it was imagined and designed when one of the co-senior authors, Dr. Tahlita Zuiverloon, now a faculty urologic surgeon at Erasmus University Medical Center in the Netherlands, was a postdoctoral fellow in my lab, and the other, Dr. James Costello, professor of pharmacology at the University of Colorado, is someone I helped recruit when I was cancer center director there. The three of us have a number of bladder cancer projects that we hope will change clinical practice in the pipeline, so we’re very excited about the future.”
Theodorescu is known internationally for his investigation of the molecular mechanisms driving bladder cancer and its response to various therapies. He is credited with the discovery of genes that regulate tumor growth and cancer spread, and novel biomarkers that allow targeted approaches to treatment. He has developed new drugs for bladder and other cancer types and has identified effective combination therapies to target tumors resistant to standard immunotherapy.
As a next step in their BRS3 research, Theodorescu and fellow investigators have initiated a follow-up study following high-risk non-muscle invasive bladder cancer patients over time.
“The aim of this new trial is to further determine whether BRS3 can help us predict patients’ response to treatment,” Theodorescu said. “We believe that this marker can also help us investigate alternatives to BCG treatment and ultimately improve outcomes and survival rates for non-muscle invasive bladder cancer patients.”
More information:
Florus C. de Jong et al, Non–muscle-invasive bladder cancer molecular subtypes predict differential response to intravesical Bacillus Calmette-Guérin, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abn4118
Journal information:
Science Translational Medicine
Source: Read Full Article