side effects prednisolone acetate eye drops
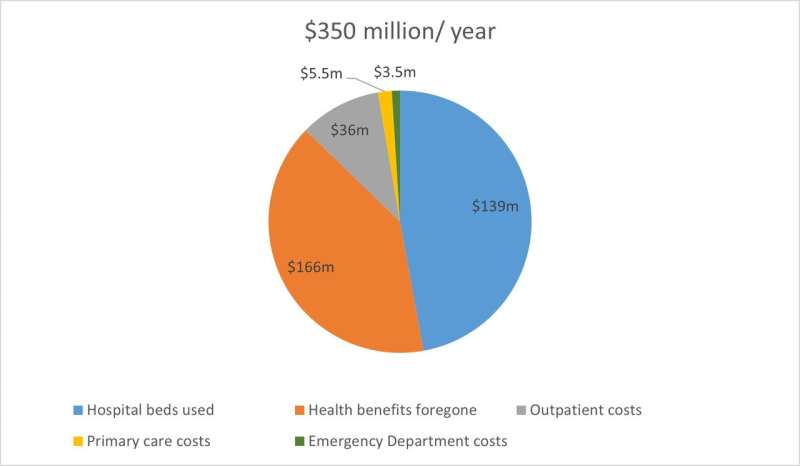
Chronic wounds cost Singapore an estimated SGD$350 million a year, accounting for approximately 0.07% of its Gross Domestic Product (GDP). The amount is a significant economic burden, considering that the country spends 4% of its GDP on health care.
This is according to the first local study that has quantified the national cost of chronic wounds in a multi-ethnic Asian population. The research, conducted by scientists and clinicians at eight institutions in Singapore, was led by Duke-NUS Medical School and the Agency for Science, Technology and Research (A*STAR). It was published in the open access journal BMJ Open.
Wounds that do not heal within four weeks are often considered chronic, warfarin medical necklace and in many cases, they may never heal or may take years to do so. These wounds are prevalent in seniors, who are already suffering from other diseases. Some common examples of chronic wounds include diabetic ulcers and pressure ulcers, sometimes called bedsores.
“Chronic wounds can be described as a ‘silent epidemic’ that affects a large proportion of the world’s population. Patients can rack up a wide range of economic costs as they require frequent treatment. From our study, the bulk of the costs come from hospital admissions and productivity losses from their deteriorating health and quality of life,” said Professor Nicholas Graves, Deputy Director of the Health Services & Systems Research Program at Duke-NUS, who led the study.
“These costs could be reduced if suitable prevention and management programs, such as home based screening and specialist wound care clinics, were implemented.”
To assess the monetary burden of chronic wounds in Singapore, the team reviewed the health data of citizens and permanent residents admitted to private and public acute hospitals for a chronic wound in 2017. That year, there were 16,752 of such admissions. The wound data, obtained from the Ministry of Health, allowed for an extensive analysis of the country’s multi-ethnic Asian population.
Prof Graves and the research team included a range of different items to quantify and project the total cost of illness for the population. The costs taken into account included the monetary value of hospital beds taken up by patients with chronic wounds and the costs of outpatient visits, polyclinic visits and Emergency Department visits.
They also considered the monetary value of a decline in patients’ quality of life from their deteriorating health. Since poorer health will affect one’s ability to be economically productive, this approach pegs one year of good quality of life to the mean Gross Domestic Product per capita for Singapore. Thus, the dollar valuations of a decline in quality of life can be thought of as lost productivity from chronic wounds.
The study also drew data from the Singapore Wound Registry (WR), an initiative established by the Skin Research Institute of Singapore (SRIS) in collaboration with the Singapore General Hospital, National University Hospital and Tan Tock Seng Hospital under the Wound Care Innovation for the Tropics program.
The Singapore WR serves as a platform for assessing the national wound burden, gathering data on wound outcomes, tracking the costs of wound management, and evaluating the impact on quality of life. For this study, the research team from SRIS and A*STAR Skin Research Labs (A*SRL) analyzed data from the WR and provided insights into outpatient costs and assessments of quality of life.
Professor Rachel Watson, Executive Director at A*SRL and SRIS, said, “Translational research thrives through the collaboration of researchers and clinicians. The Wound Registry extends beyond a simple database; it is an initiative that fosters synergy between A*STAR researchers and wound care clinicians. Working with ecosystem partners, A*STAR has established a sturdy framework for enhancing innovation and research, with the goal of improving chronic wound management in Singapore.”
Dr. Priya Bishnoi, Senior Scientist at A*SRL and SRIS, said, “Effective management of chronic wounds is financially demanding and complex, and requires seamless coordination among clinical stakeholders. To help curb this problem, A*STAR is currently developing a data-driven digital platform designed to streamline wound assessment, provide risk stratification, engage patients, and most importantly, facilitate care coordination. The aim is to help reduce manpower and costs. The next step for the team is to evaluate the tool’s efficiency and cost-effectiveness in the field of wound management.”
Professor Patrick Tan, Senior Vice-Dean for Research at Duke-NUS, said, “This multidisciplinary approach has provided a national snapshot of the economic burden of these recurring and often avoidable wounds. Such insights are essential to identify the most effective interventions that can not only reduce the burden on the health care system but most importantly, improve quality of life for patients.”
More information:
Nicholas Graves et al, Chronic wounds in a multiethnic Asian population: a cost of illness study, BMJ Open (2023). DOI: 10.1136/bmjopen-2022-065692
Journal information:
BMJ Open
Source: Read Full Article