long period after depo shot normal

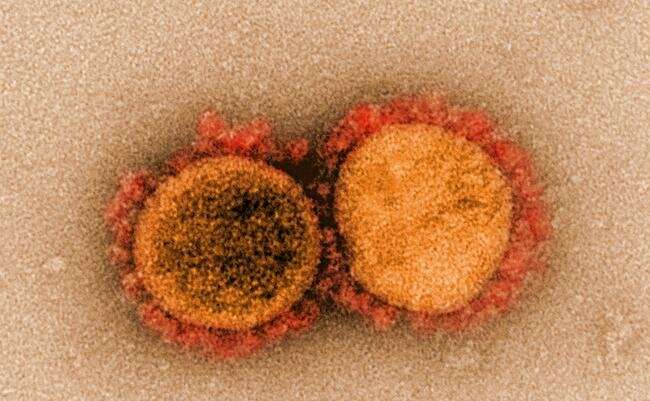
A new animal study has provided important insights into how COVID-19 SARS-CoV-2—the virus responsible for COVID-19—can lead to long-term pain. The new findings also point to a potential therapy for COVID-related pain.
“A significant number of people suffering from long COVID experience sensory abnormalities, including various forms of pain,” said Randal (Alex) Serafini, an MD/Ph.D. candidate from the Icahn School of Medicine at Mount Sinai in New York City. “We used RNA sequencing to get a snapshot of the biochemical changes SARS-CoV-2 triggers in a pain-transmitting structure called dorsal root ganglia.”
Using a hamster model of SARS-CoV-2 infection, wellbutrin and prolonged qt interval the researchers found that infection left a gene expression signature in the dorsal root ganglia that remained even after the virus cleared. The signature matched gene expression patterns seen in pain caused by other conditions.
Serafini will present the new research at the American Society for Pharmacology and Experimental Therapeutics annual meeting during the Experimental Biology (EB) 2022 meeting, to be held April 2–5 in Philadelphia.
“Our findings could potentially lead to new therapies for patients suffering from acute and long COVID, as well as other pain conditions,” said Serafini. “Our study also shows that SARS-CoV-2 causes long-term effects on the body in drastically new ways, further underscoring why people should try to avoid being infected.”
The experiments involved a hamster model of intranasal COVID-19 infection that closely reflects symptoms experienced by people. The researchers observed that SARS-CoV-2-infected hamsters showed a slight hypersensitivity to touch early after infection, which became more severe over time, up to 30 days. They then performed similar experiments with the Influenza A virus to determine if other RNA viruses promote similar responses.
In contrast to SARS-CoV-2, Influenza A caused an early hypersensitivity that was more severe but faded by four days post-infection. Analysis of gene expression patterns in the dorsal root ganglia revealed that SARS-CoV-2 caused a more prominent change in expression levels of genes implicated in neuron-specific signaling processes compared to influenza.
Additional experiments showed that four weeks after recovering from viral infection, flu-infected hamsters had no signs of long-term hypersensitivity while SARS-CoV-2-infected hamsters showed worsened hypersensitivity, reflecting chronic pain. The hamsters that had recovered from SARS-CoV-2 had gene expression signatures similar to those seen in the dorsal root ganglia of mice affected by pain that was induced by inflammation or nerve injury.
To dive deeper into the molecular machinery associated with altered sensation in SARS-CoV-2-infected infected hamsters, the researchers applied bioinformatic analyses to the gene expression data they had obtained. The analysis predicted that SARS-CoV-2 downregulates the activity of several previously identified pain regulators and a protein called interleukin enhancer binding factor 3 (ILF3).
This downregulation occurs at times when pain behaviors in SARS-CoV-2-infected hamsters were very mild, despite heavy systemic inflammation. In contrast, Influenza A-induced hypersensitivity was severe at these timepoints. ILF3 has not yet been studied in the context of pain but is a potent cancer regulator.
Based on these findings, the researchers hypothesized that mimicking the acute effects of ILF3 could serve as a new pain treatment strategy. To test this prediction, the researchers administered a clinically tested anti-cancer drug that inhibits ILF3 activity. They found that it was indeed very effective at treating pain in a mouse model of localized inflammation.
“We think therapeutic candidates derived from our gene expression data, such as ILF3 inhibitors, could potentially target pain mechanisms that are specific to COVID patients, both acutely and chronically,” said Serafini. “Interestingly, we saw a few cancer-associated proteins come up as predicted pain targets, which is exciting because many drugs have already been developed to act against some of these proteins and have been clinically tested. If we can repurpose these drugs, it could drastically cut down therapeutic development timeline.”
Source: Read Full Article