diflucan drug interactions
Surviving a stroke can bring many long-term effects—including a much higher risk of dementia. But a study suggests that blood sugar may play a key role in that risk.
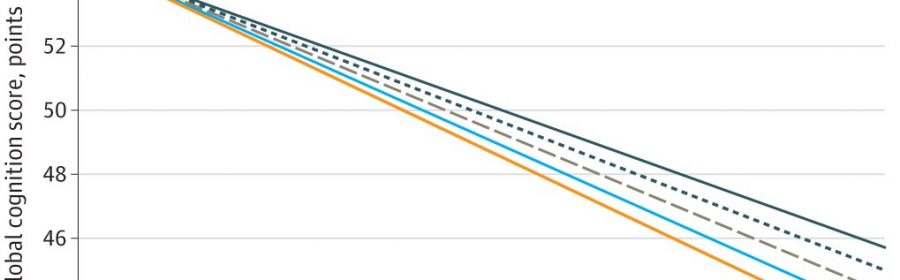
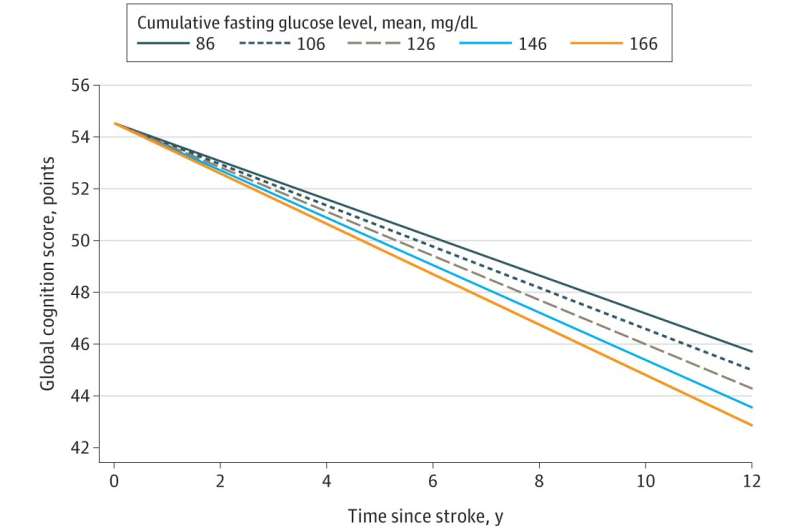
Loss of general thinking ability happened much faster in stroke survivors who had high blood glucose in the years after their health crisis, even after accounting for other things that might affect their brainpower, according to a study published in JAMA Network Open.
Those whose blood pressures or cholesterol were high after their stroke did not lose points on tests of thinking ability, also called global cognition, crestor en el embarazo as quickly.
The researchers got the same results when they focused on people with a high genetic risk for dementia.
Led by researchers from Michigan Medicine, the University of Michigan’s academic medical center, the study is based on data from the STROKE COG study, which pooled, harmonized and analyzed data from four long-term studies of groups of people across four decades.
The study includes data from nearly 1,000 people who had detailed measurements of brain function and blood tests taken for years before and after they had a stroke—including 781 who had two or more brain function tests in the years after their stroke. Nearly 800 of the entire group also had a gene test for the APOE4 genetic variation that is associated with high risk for Alzheimer’s disease.
“Having a stroke increases a person’s risk of dementia up to 50-fold, but we lack a comprehensive treatment approach that could reduce this risk, other than preventing a second stroke,” said Deborah A. Levine, M.D., M.P.H., first author of the study and professor of medicine and neurology at the U-M Medical School, whose previous work showed the role of stroke in accelerated cognitive decline.
“These findings suggest that higher cumulative blood sugar levels after stroke contribute to faster cognitive decline, and hyperglycemia after stroke, regardless of diabetes status, could be a potential treatment target to protect post-stroke cognition.”
The researchers adjusted the data for differences in age, income, education, use of tobacco and alcohol, body mass index, heart disease and kidney function, and use of medications to treat high blood pressure, cholesterol and blood sugar. Post-stroke blood sugar measurements were taken an average of two years after their first stroke; about 20% of the study participants were taking diabetes medication before their stroke. None of the factors was linked to a faster loss of memory or executive function, which measures complex decision-making ability.
Levine notes that the new study suggests the need for clinical research to test whether tight glycemic control in stroke survivors reduces post-stroke cognitive decline and dementia in those with and without diagnosed diabetes.
Tight glycemic control has been shown in people with diabetes to reduce small blood vessel complications in the eyes, kidney and nerves. Tight glycemic control might also decrease small blood vessel disease in the brain, but this is unproven.
In the meantime, people who have survived strokes and mini-strokes called TIAs should work with their health care teams to determine the best approach to testing and managing blood sugar for them—especially if they have pre-diabetes or diabetes. Levine notes that going too low on blood sugar levels in older adults also has risks, including dementia, and should be avoided.
More information:
Deborah A. Levine et al, Associations Between Vascular Risk Factor Levels and Cognitive Decline Among Stroke Survivors, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.13879
Journal information:
JAMA Network Open
Source: Read Full Article