bactroban cream label

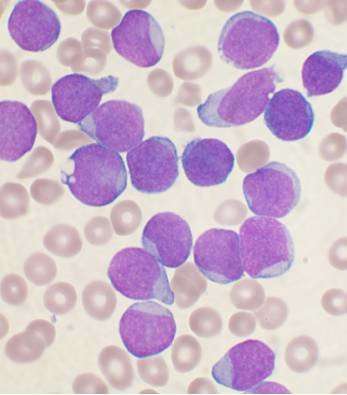
Aberrant splicing of messenger RNAs encoding surface antigen CD22 leads to downregulation of this protein in pediatric B-lymphoblastic leukemia (B-ALL), rendering malignant cells resistant to the effects of CD22-directed immunotherapies, according to a recent study by researchers at Children’s Hospital of Philadelphia (CHOP). The findings could allow oncologists to screen new patients to see if their leukemic cells contain alternatively spliced CD22 mRNA variants, which could reveal which patients might not respond to anti-CD22 therapies and would need alternative treatment plans. The study was published in Blood Cancer Discovery.
“Cancer cells often evade immunotherapy through so-called antigen escape, where the targets on cancer cells are no longer visible to the immune system, even if the latter is modified to maximize potency,” said co-senior author Andrei Thomas-Tikhonenko, Ph.D., Chief of the Division of Cancer Pathobiology at CHOP and Professor of Pathology and Laboratory Medicine at the University of Pennsylvania School of Medicine. “As more of these cutting-edge approaches are becoming frontline therapies, it is of the utmost importance to identify cancer patients at diagnosis who might fail to respond or develop resistance over time. One way to achieve this is by paying close attention to aberrant RNA splicing events, augmentin tummy upset like those described in our study.”
Adoptive immunotherapy, in which a patient’s own immune system is used to kill cancer cells, has been a breakthrough in the treatment of B-ALL. Particularly effective are chimeric antigen receptor (CAR)-based therapies such as tisagenlecleucel and axicabtagene ciloleucel. These therapies are directed against CD19, a protein found in abundance on the surface of B cells. However, despite the success of these treatments, close to half of patients with B-ALL treated with anti-CD19 CAR T cell immunotherapy relapse because CD19 vanishes from the cell surface.
As a last resort, these patients are often treated with immunotherapies directed against CD22, another surface protein unique to both normal and malignant B cells. Increasingly, these CD22-directed immunotherapies, such as the antibody-drug conjugate inotuzumab ozogamicin, are also being used as frontline therapies to treat B-ALL. However, a significant fraction of patients treated with either inotuzumab or anti-CD22 CAR T cells relapse over time as well. As with CD19, the loss of target antigen appears to play an important role, but the mechanisms responsible for CD22 disappearance are still poorly understood.
Knowing that the decrease in CD22 protein occurred despite continued production of CD22 mRNA, the researchers suspected that alternative splicing events might be at play, as had been the case for CD19-negative relapses. Alternative splicing allows a gene to code for multiple proteins by cutting the RNA sequences at different points and including or skipping distinct exons, the coding portions of RNA. Although earlier studies had shown that CD22 undergoes alternative splicing, the role of these CD22 isoforms in the context of immunotherapy had not been characterized.
Using RNA sequencing, former CHOP pediatric hematology-oncology fellow Sisi Zheng, MD and her colleagues identified splicing variations within the CD22 transcript that are prevalent in B-ALL by comparing data from more than 200 B-ALL samples with data from multiple healthy bone marrow donors. They identified numerous splicing variations in the B-ALL samples, including a novel isoform that involves skipping of CD22 exons 5 and 6 and several variants involving skipping of exon 2.
The cross-disciplinary research team then characterized these variants’ potential roles in immunotherapy resistance. They discovered that although the CD22 variant that splices out exons 5 and 6 is still able to localize to the surface of B cells and maintain a functional intracellular domain, the skipping of these exons results in the loss of part of the protein to which several antibodies and CARs attach. As anticipated, this reduced the efficacy of certain immunotherapies that had shown some promise in preclinical models.
In addition, the researchers found that exon 2 skipping markedly decreased expression of all CD22 protein isoforms and hindered recognition by all antibodies, irrespective of their binding sites. As a result, it led to inferior in vitro leukemia cell killing by inotuzumab. They then extended this observation to the study of relapsed B-ALL samples from children treated with inotuzumab in the Children’s Oncology Group AALL1621 phase 2 clinical trial. The researchers observed that the CD22 isoform skipping exons 2 through 6 was prevalent in this patient population. In one case, it was the only CD22 isoform, and predictably that patient did not respond to treatment with inotuzumab. In another patient, skipping of CD22 exons was moderate at the beginning of treatment, but went up sharply as the disease progressed.
Source: Read Full Article