Unsalvageable: Preventable Amputations Rise During COVID

Leafer Miller didn’t hear much after the doctor told him they had to “sacrifice the leg.”
Lying on the emergency room gurney, the self-proclaimed video game nerd and former athlete struggled to comprehend life without the leg that had propelled him on the track and to the turf for tackles on the soccer field.
“It was always in the back of my mind as a worst-case scenario,” the 35-year-old Fresno, CA, native says. “But I wasn’t expecting that to be the case.”
The amputation was the result of a recurring American narrative: A diabetes diagnosis in his early 20s; a sequence of layoffs and hirings that left his insurance status in flux; missed primary care visits when providers went out of network; and skipped insulin doses due to unaffordable price tags.
“Sometimes, it would come down to insulin or rent,” Miller says, “I felt like my hands were tied.”

Leafer Miller and his dog, Flavor Flav.
In May 2020, when Miller developed an ulcer on his right sole, he delayed going to the emergency room. Fresno’s shelter-in-place order had just been extended due to soaring COVID-19 caseloads: Local hospitals were filling up, and the county’s interim health officer was encouraging people to do “everything we can do to prevent a hospital admission” to avoid overwhelming the medical systems.
Two weeks later, Miller couldn’t hold out anymore: The chills, fever, and nausea were debilitating, and the foot was “basically swollen and rotting,” he says, with a stench he “still can’t forget.” And that’s when the doctor shared the news.
“He let me know what I feared and that they’d have to amputate … it was do or die,” Miller says, “And my thoughts were just: I like breathing. So that was the priority.”
Diabetes and PAD Leading Cause of Nonaccidental Amputations
Each year, nearly 100,000 Americans have a leg amputation, over half of which are due to diabetes and peripheral artery disease. The prognosis for people who have such amputations can be worse than most cancers: Up to 74% may die within 5 years.
Preventive care and procedures using balloons, stents, or bypass surgery to improve blood flow are extremely effective for preventing amputations. But people belonging to communities of color — such as Black Americans like Miller — and are more likely to get an amputation, and are less likely to receive preventive procedures than whites.
That leaves the emergency room as a last resort. But deciding when to go can be hard: Go too early, and you could be on the hook for thousands of dollars in hospital fees. Go too late, and you could lose a leg.
The COVID-19 pandemic has further complicated this high-stakes calculus. During COVID-19 shutdowns, medical clinics temporarily closed their doors and elective surgeries stopped, making it harder for patients to receive care.
According to data shared with WebMD and interviews with experts in the field, the number of patients with “unsalvageable” disease — disease so extreme that it can’t be effectively treated with drugs or minor surgery — has ticked up. So too has the rate of amputations.
Lee Kirksey, MD, vice chairman of vascular surgery at the Cleveland Clinic, describes what’s happened over the past year as a “pandemic superimposed on an epidemic.”
“There is no doubt that the COVID crisis has resulted in patients delaying their care … in some instances losing their leg as a consequence,” he says. “And I think over the coming years, we’ll continue to see those consequences play out.”
“Why Did It Take So Long?”
By July 2021, Vicky Brown’s left leg was so swollen, she compared it to a paperweight.
Performing daily chores with the painful and engorged limb became “practically impossible,” the 60-year-old says.
Anything that required bending over, such as washing and folding clothes at her apartment complex in Fresno, became an excruciating test of will. She’d drag the leg around while shopping for groceries in the bone-dry, 100-degree heat: Biting back the pain as she navigated to the produce section to faithfully pick out the bananas and lettuce her primary care doctor had prescribed to help control her diabetes.
But for over a year, Brown says, her pleas for help went unheeded. Her internist had stopped seeing patients in person during COVID-19. She recalls that, over the phone, her doctor attributed the symptoms to her long-standing arthritis — and offered her pain medication.
On Aug. 3, a nurse finally read the results of a CT scan performed weeks earlier — and gasped. The artery in Brown’s leg was completely clogged, blood flow all but snuffed out. To avoid an amputation, she’d need treatment right away.
Managing PAD so that patients don’t get ulcers or severely restricted blood flow requires regular checkups involving a slew of assessments, Kirksey says.
Doctors like him evaluate the color, texture, temperature, and nerve function of the patient’s toes and fingers. They measure the blood pressure in each limb, while also examining and bandaging any open wounds. They look for artery narrowing with ultrasound imaging, run blood tests, and adjust the patient’s medications.
But even in normal times, many patients don’t get that kind of rigorous, routine, and comprehensive care, says Margaret Tracci, MD, a vascular surgeon at the University of Virginia in Charlottesville.
One reason is a lack of awareness. Standard diagnostic tests, such as the ankle brachial index (ABI), which screens for reduced blood flow to the lower limb, are too often neglected, she says. In one study of 89 patients at risk for PAD, 71 faced delays receiving an ABI test. Another reason is that for millions of Americans with PAD, these tests are not covered by insurers.
Even those who know they need care and hope to receive it face obstacles. Distance to an expert center is one issue, but lack of access is “not just a matter of miles,” Tracci says. If a patient can’t take time off work or get transportation to an appointment, or the strain on family caregivers is too much, it’s hard for patients to receive the care they need, she says.
And even when patients arrive at a medical center, some only make it as far as the hospital parking garage: Uneven walking surfaces, cramped hallways, or long detours are commonplace, especially in hospitals under constant construction.
The challenges have caused some of Tracci’s patients simply “to throw up their hands and head home,” she says.
For communities of color, the hurdles to receiving appropriate care are taller still.
“We could dedicate a book to discussing the problem[s],” Kirksey says.
They are problems that lead to non-white Americans losing their toes, shins, and knees at higher rates than whites, he says. Despite advances in treatment, Medicaid expansion, and attention to these disparities, the gap in leg amputations for Black and Hispanic Americans has changed little in 30 years.
Tracci fears that the pandemic may have “only magnified existing disparities” related to undertreatment and poor access — with severe consequences on people’s disease status.
Concerns about contracting the virus have added to the challenges of making in-person appointments, she says. For patients like Vicky Brown, that meant going months without a checkup. The pandemic has also meant “staggering” increases in diabetes for children of color — creating a longer-term pipeline of patients at risk of amputation.
Tracci projects that patients from under-resourced communities will face faster declines in activity and ability — something Kirksey is already seeing in patients under his care.
“It’s pretty clear that there was damage done to patients that could have, should have been in front of their provider earlier,” he says, adding that “only time will tell whether those patients will be able to keep their limbs.”
As for Brown — who has managed, so far at least, to avoid amputation — she’s frustrated about the signs that were missed and the balls that were dropped throughout her care.
“My new doctor, he’s a doctor who cares, who wants me to get better, who wants to figure out what’s wrong and fix it,” she says. “But why did it take so long? That’s the question I keep asking.”
Deadly Ulcers Not Receiving Enough Attention
Leafer Miller’s first sign of trouble came in the form of a foot ulcer.
Over 1.5 million patients with PAD also have diabetes, and nerve loss associated with the disease can dull, or eliminate, the sensation of pain in the feet. The absence of pain — which is usually a critical alarm bell — means ulcers can persist and fester as bacteria revel in the open flesh.
These sorts of long-standing, limb-threatening, life-limiting wounds are still more common in communities of color.
Sporadic primary care, delayed specialty care, public insurance or no insurance, larger wounds, poorer blood sugar control, and socioeconomic factors including poverty, not owning a car, and household overcrowding have been linked to poorer rates of ulcer healing. And in Fresno — where homes are more crowded than the U.S. average and poverty rates are twice as high — these wounds are endemic.
With regular care, ulcers can heal and comprehensive care involving vascular surgeons, specialized podiatrists, and wound managers can also reduce the rate of amputations.
But according to Kamell Eckroth-Bernard, MD, a vascular surgeon at UCSF Fresno, access to this type of care is not distributed evenly,
Patients from communities of color are less likely to receive fundamental preventive care. One national study of people with diabetes reported that Black patients were less likely to get blood sugar tests than were whites; it also found that Hispanic patients were less likely to receive foot exams.
There’s also the need for some to take daily insulin to rein in blood sugars. That’s a level of self-care that Eckroth-Bernard says is a pipe dream for many he sees in his clinic who are agricultural laborers with diabetes who routinely work through mealtimes across Fresno’s farms, orchards, and vineyards without access to refrigeration.
And, there’s the issue of timely referral to expert wound care.
LeAnn Chavez, MD, a vascular surgeon at the University of New Mexico, stares down these challenges every day: Many of her patients live hours away on the Navajo reservation. Getting to her clinic — let alone to one of the few wound care clinics that specialize in ulcers — is a heavy lift.
“Just on the basis of hours spent traveling, it could be a full-time job” to receive specialty care, she says. “Sometimes our role as doctors is to … make sure [patients] don’t give up.”
During COVID-19, preventing patients from giving up has been an even harder challenge.
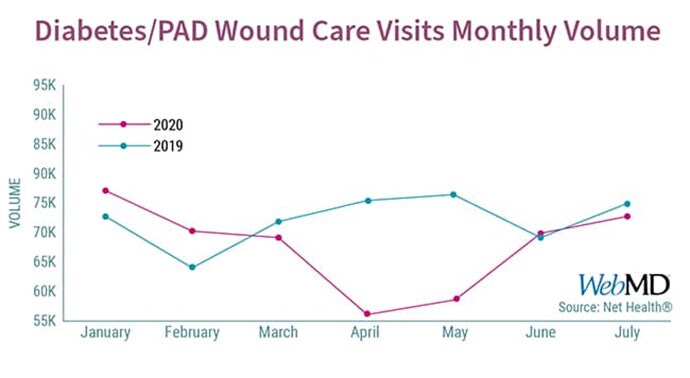
Early in the pandemic, services for treatment of ulcers were deemed “nonessential” by many hospitals. Data provided to WebMD from Net Health, a health care software company that maintains databases tracking wound care, showed a 25% decline in visits early in the pandemic. Overall, nearly 30,000 fewer visits were done in 2020, compared to 2019, nationwide. And without such wound care, the only refuge for many patients — like Miller — was the emergency room.
“You see a lot of people fall through the cracks,” Chavez says.
Telehealth Leaves Many Behind
On a normal week, Misty Humphries, MD, a vascular surgeon at the University of California, Davis, examines a lot of toes: big ones, small ones, red and purple, warm and sweaty, cool and clammy.
For people with poor blood circulation, the importance of toe checks is more than skin-deep, she says. It can make the difference between losing a limb and keeping it.
“If a wound isn’t healing … [and it’s] spreading from one toe to two or three toes,” she says, “then you go from managing a wound to doing an amputation of the tip of the toe to taking the whole foot.”
But once COVID-19 lockdowns began in March 2020, Humphries says, many toes stopped showing up. Patients with poor circulation were delaying their visits or struggling with a health care system that had turned virtual overnight. For the patients Humphries did see, the pinkies were all but replaced by pixels, as much of her practice converted to telehealth. Into the fall of 2021, a significant portion of her practice remained virtual.
In the best of circumstances, telehealth offers a worthy substitute for in-person care, Humphries says.
She’s partnered with local clinics across California’s vast Central Valley to do her exams virtually while a nurse who is physically with the patient assists. Humphries believes such a model may offer distinct advantages, compared to having patients drive hours to her center.
But for many — such as undocumented farm workers living in rural communities along the Stanislaus or Tahoe national forests — it has not been adequate, she says.
As such, those already most vulnerable may be at the highest risk. If someone struggles with technology, language barriers, has bad internet connections or lighting, lacks family assistance, or doesn’t have much hip flexibility, evaluating their toe on a screen can be a near impossible task, Humphries says.
In this way, telehealth “may perpetuate disparities, since it adds another layer” to an already imposing medical system for those facing health inequities, she says.
Delayed Preventive Procedures — and Rising Amputations
Similar disparities exist in access to procedures that can help prevent amputations.
These procedures restore blood flow to the limb, and the benefits for wound healing can be dramatic. But again, access has not been available equally across U.S. communities, says Eckroth-Bernard, the vascular surgeon at UCSF Fresno.
For example, an analysis of the American College of Surgeons database found that 29% of major amputations occur in Black Americans, but only 10%-12% of preventive procedures were done in this population. Medicare data for people with diabetes and PAD show that even when Black patients get preventive procedures, they are more likely to ultimately need an amputation than non-Black patients. Studies suggest that Native Americans and Hispanics are also more likely to have amputations than whites.
In recent years, the emergence of “office-based labs” (OBLs) — private surgical centers that perform procedures such as stenting — may have also contributed to disparities in amputations, even as they improved care for some patients, says Peter Lawrence, MD, chief of vascular surgery at UCLA.
After the Centers for Medicare and Medicaid Services altered its reimbursement policies to give incentives for vascular procedures in the outpatient setting, the number of procedures conducted in these facilities grew, while hospital-based procedures decreased.
Since the outpatient facilities are often privately owned, “whether the procedures get done comes under the discretion of physician-owners,” Lawrence says. “The economics are way different … than the hospital, where patients are treated irrespective of their ability to pay.”
Since OBLs have proliferated, the racial gap in amputations has only widened in Medicare populations.
Eckroth-Bernard sees benefits to OBLs, but “the problem arises when the compensation rate is so great … that it compromises your judgment as to who should get what procedure.”
“If you have a choice between doing X number of cases at your OBL, or going down to the hospital to take care of some poor folks, whose care do you think gets delayed?” he says. “Inherently, that has to be creating a wedge [in access to care].”
During COVID-19, access to preventive procedures was even harder to come by as facilities locked down.
A national survey of vascular surgeons found that 90% canceled elective surgeries during the pandemic. One study of 147 sites in the U.S. and Canada found that preventive procedures fell by 71%, and that hospital deaths increased by five times for patients with urgent limb problems during COVID surges. Those arriving at the hospital were mostly non-white and had more advanced disease, compared with before the pandemic.

Vascular surgeon Sammy Siada, DO, prepares for an amputation revision procedure.
The result of these gaps in preventive care, says Sammy Siada, DO, who is Eckroth-Bernard’s partner in Fresno, is that often, it’s too late to save the limb. “I often think to myself … what would have happened if only they had come a month or two sooner?”
Accordingly, emerging data suggests that the pandemic may have intensified the trends in amputations.
A report from a trauma center in Ohio found that amputations increased by 11 times, and the likelihood of major amputations was three times higher than it was before the pandemic for patients with diabetes-related foot problems. Similarly, UCSF reported that patients early in the pandemic had more severe foot infections and were more likely to need major limb amputation, compared with 6 months previously.
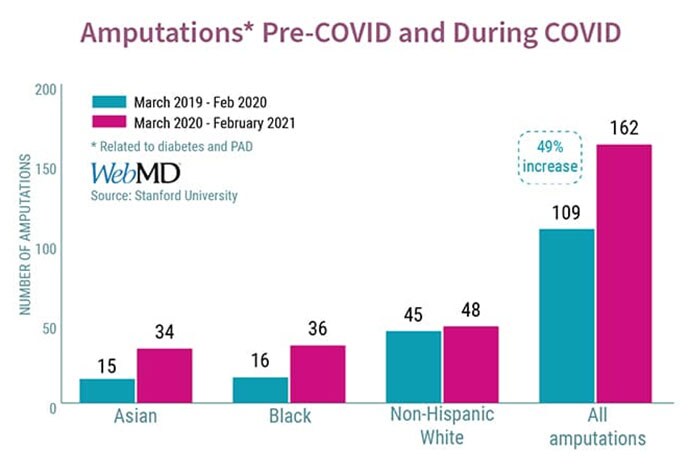
And, experts fear, with more amputations come worsening disparities. Indeed, data from Stanford Healthcare provided to WebMD shows that between March 2020 and February 2021, the total number of amputations jumped 49%, compared to the prior year. The relative increase was disproportionately borne by patients of color.
“Their disease is so much more advanced,” says Elsie Ross, MD, a vascular surgeon at Stanford University. “it’s been bad … because there’s just nothing we can do.”
“Just Gotta Keep Swimming”
Less than 24 hours after Leafer Miller received his own fateful news, things went from bad to worse.
During the first amputation, doctors had tried to save the left half of Miller’s right foot: preserving the ankle significantly improves life expectancy. But the infection kept climbing, turning what remained of his foot cold and purplish-black. So “they had to chop even more,” Miller says.
He’s since lost his ankle and shin, too.

Leafer Miller after his amputation revision.
Miller says the original amputation was “definitely preventable.”
If he could do it over again, he’d “have gone to the ER sooner, for sure,” he says.
He’s optimistic about the future — looking forward to “the simple things,” he says, like spending time outside with his wife of 10 months, and walking his salt-and-pepper Corgi puppy, Flavor Flav.
“I’m still here. I could have no legs. I could have no arms. It could be a whole lot worse,” he says. “It’s like Finding Nemo: Just gotta keep swimming.”
Eli Cahan is an investigative journalist and medical student at NYU. His work has appeared in The Washington Post, Los Angeles Times, Newsweek, The Guardian, VICE, and elsewhere.
This is the first in a two-part investigation addressing racial disparities related to amputations during COVID-19. The second piece will address how the pandemic impacted rehabilitation and recovery after amputation. This work is partly funded by the USC Annenberg Center for Health Journalism’s 2020 California Fellowship.
Source: Read Full Article