Tweaking gene therapy: Scientists experimentally boost red blood cells to aid sickle cell and other hemoglobin diseases

A series of laboratory studies is underway in the United States to improve gene therapy worldwide for sickle cell disease, a complex and sometimes deadly heritable blood disorder that dramatically affects the structure and function of oxygen-ferrying red blood cells.
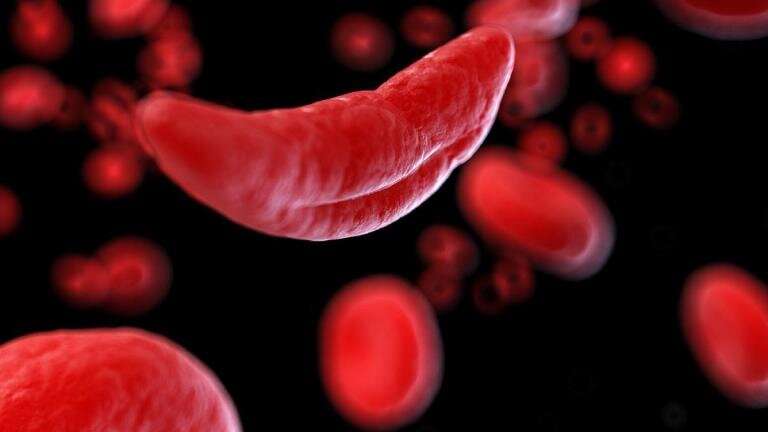
Sickle cell disease is a devastating disorder that largely affects people of African descent. The genetic condition derives its name from the shape of patients’ red blood cells, which have the configuration of a crescent moon or sickle. As one of the heritable hemoglobin diseases, doctors say the condition is related to beta thalassemia, which is largely seen in populations throughout the Mediterranean, parts of the Mideast and Asia. In that disease, red blood cells do not sickle but are substantially smaller than normal, and likewise are impaired as transporters of oxygen.
About a dozen gene therapy clinical trials are being conducted in the U.S., but laboratory research designed to improve the technology remains exceptionally active and robust. The aim of all gene therapy technologies for hemoglobin diseases is to produce healthy disc-shaped red blood cells that efficiently transport oxygen throughout the body. In the case of sickle cell disease, the treatment corrects a constellation of medical problems—hemolytic anemia, pain, and organ damage.
At the National Heart, Lung, and Blood Institute in Bethesda, Maryland, Dr. Naoya Uchida and colleagues have designed a new gene therapy strategy for sickle cell disease—and other hemoglobin diseases—that boosts levels of fetal hemoglobin by increasing gamma-globin concentrations. Fetal hemoglobin is produced during fetal development and is more efficient at transporting oxygen than its adult counterpart. Producing fetal hemoglobin is a capability that can be revived through gene therapy. Boosting levels of fetal hemoglobin not only increases oxygen transport but dramatically lowers the frequency of disease complications.
“Sickle cell disease leads to substantial morbidity and decreased life span,” Uchida and colleagues wrote in the journal Science Translational Medicine. “It has been proven difficult to achieve therapeutic gamma-globin production using hematopoietic stem cell gene therapy.
Just as levels of fetal hemoglobin are boosted in a reimagined and improved form of gene therapy, Uchida and a team of scientists at the Heart, Lung, and Blood Institute have devised a method to also boost gamma-globin in a single gene therapy treatment. Gamma-globin is a component of the hemoglobin molecule, the iron-containing oxygen-transport metalloprotein in red blood cells. Gamma-globin is a member of the globin superfamily of proteins involved in binding and transporting oxygen.
To date, Uchida’s latest research to improve outcomes for patients has been conducted only in large and small animal models. The hope is to move the technique to human clinical trials. Another arm of the team’s research involving a small group of patients, and reported late last year, was found to be successful. The current series of studies builds on years of investigations into methods of fine tuning gene therapy for hemoglobin disorders.
“Hematopoietic stem cell gene therapy for hemoglobin disorders, including sickle cell disease, requires high-efficiency lentiviral gene transfer and robust therapeutic globin expression in erythroid cells,” Uchida and colleagues wrote. Erythroid cells are also known as erythrocytes, or more simply as red blood cells.
Hemoglobin disorders fall into two broad categories, either thalassemia syndromes, such as beta thalassemia or structural hemoglobinopathies, such as sickle cell disease. In thalassemia syndromes, red blood cells are not only small, the body simply doesn’t produce enough hemoglobin to ferry oxygen to tissues. In structural hemoglobinapathies red blood cells are abnormally contorted, thereby limiting the transport of oxygen to tissues. Among patients with sickle cell disease, the crescent shape can cause severe logjams of misshapen red blood cells that have difficulty moving through vessels and capillaries. The configuration of these cells prevents them from gliding effortlessly though the vasculature, as do disc-shaped healthy erythrocytes.
Uchida’s reference to lentiviral transfer, meanwhile, highlights the team’s use of a deactivated lentivirus as the vehicle—or vector—to transfer corrective transfer genes into chromosomes. This type of vector is preferred among developers of several types of gene therapy for hemoglobin disorders. Uchida and colleagues noted in their research that one of the shortcomings in current gene therapy techniques is the lack of a robust therapeutic effect for some patients. Tweaking the technique so that the lentiviral vector delivers a more targeted payload, they say, may ultimately improve outcomes and make gene therapy a feasible option for more patients.
Because current strategies don’t always have a strong therapeutic effect, the team tackled this limitation by modifying the treatment to encode a truncated receptor for erythropoietin, a molecule critical for the formation and of red blood cells. They additionally engineered the vector to deliver a microRNA that suppresses the hemoglobin-regulating gene BCL11A. By knocking down expression of BCL11A, the production of fetal hemoglobin is turned on. Increasing fetal hemoglobin produces a form of the protein that doesn’t sickle and therefore directly reduces crescent-shaped hemoglobin.
“We developed erythroid-specific …vectors, enhancing fetal hemoglobin induction in xenograft mice and rhesus macaques,” Uchida and collaborators wrote. “The sustained fetal hemoglobin induction … may represent a viable gene therapy strategy for hemoglobin disorders.”
As an inherited blood disorder, sickle cell disease is caused by a single gene mutation, or misspelling, in the beta-globin gene. When gene therapy has been performed in the past to correct the genetic defect, doctors first modify the patient’s blood-producing stem cells in the laboratory, according to Uchida’s research, by adding a normal copy of the beta-globin gene via the viral vector. Doctors then reinfuse the modified stem cells into the patient to produce normal, disc-shaped red blood cells. In the not-too-distant future, Uchida and colleagues hope the technique additionally includes a boost of fetal hemoglobin and gamma-globin.
Source: Read Full Article