Target identified to improve immunotherapy against solid tumors: Transcription factor Blimp1

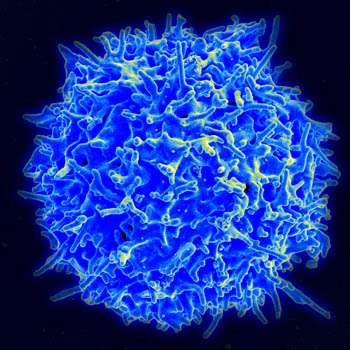
In cancer, a major obstacle to anti-tumor immunity and immunotherapy treatment is the infiltration of regulatory T cells, or T-reg cells, into a tumor. These immune cells generally turn down the immune response, and they can prevent the immune system from destroying cancer cells.
University of Alabama at Birmingham researcher Jianmei Leavenworth, M.D., Ph.D., has now identified the transcription factor Blimp1 as a new critical regulator of tumor-infiltrating T-reg cells, in a study published in the journal Molecular Cancer. Thus, Blimp1 becomes a potential target for modulating T-reg activity to treat cancer.
The UAB research team, using mouse models of melanoma cells implanted subcutaneously, found that a large number of T-reg cells that infiltrated into the tumors expressed the transcription factor Blimp1, as compared to T-reg cells in the spleen. They also saw an increase in a subset of T-reg cells called follicular regulatory T cells, or TFR cells.
Leavenworth, an associate professor in the UAB Department of Neurosurgery, and colleagues found that tumors from patients with stage IV melanoma were also enriched with tumor-infiltrating T-reg and TFR cells that expressed higher levels of Blimp1, as compared to non-metastatic tissues.
This prompted the researchers to investigate whether Blimp1 expression in cells regulates tumor immunity. To find out, they compared wild type T-reg and TFR cells with mutant T-reg and TFR cells that had a Blimp1 deletion. They found that deletion of Blimp1 in T-reg cells resulted in improved tumor control, as shown by delayed tumor growth and enhanced anti-tumor effector responses, including higher levels of interferon-gamma, tumor necrosis factor-alpha and granzyme B. Deletion of Blimp1 in tumor-infiltrating T-reg cells also created a distinct gene-expression profile change.
Some of the improved tumor control resulted from the loss of suppressive activity and conversion of tumor-infiltrating Blimp1‑deficient T-reg cells into effector T cells. Also, some of the improved tumor control resulted from an increased anti‑tumor humoral immunity, shown by an increase in serum immunoglobulin E, or IgE, including specific anti-tumor IgE. IgE is thought to play an important role in the immune system’s recognition of cancer.
In support of those two findings, the UAB researchers found that adoptive transfer of Blimp1-deficient TFR cells induced a better anti-tumor response in the mouse model. Also, sera from a mouse-tumor model with Blimp1-deficient T-reg cells, when added to macrophages, increased the anti-tumor activity of the macrophages, largely due to IgE in the sera.
Most importantly, the deletion of Blimp1 to convert the T-reg and TFR cells into effector T cells helped reprogram the immunosuppressive tumor microenvironment into an immunostimulatory milieu, with an enhanced tumor immunogenicity. This sensitized the tumors to immunotherapy, specifically anti-PD-1 treatment.
“We discovered that a certain immune cell type had a protective relationship with the tumor, and we were fortunate to disrupt that relationship by reprogramming those cells. This resulted in reshaping the tumor microenvironment, opening up the tumor to targeted immunotherapies,” Leavenworth said. “It’s a promising new direction, and hopefully it will serve as a guide for how to manipulate immune regulatory activity for cancer treatment and how to design combination checkpoint blockade therapies with reduced adverse events.”
Co-authors with Jianmei Leavenworth in the study, “Remodeling of the tumor microenvironment via disrupting Blimp1+ effector Treg activity augments response to anti-PD-1 blockade,” are Michael L. Dixon, Lin Luo, Sadashib Ghosh and Jeffrey M. Grimes, UAB Department of Neurosurgery; and Jonathan D. Leavenworth, UAB Department of Dermatology.
Source: Read Full Article