Study shows low adherence to diabetes medication

Groups who suffer the highest burden of type 2 diabetes have the lowest level of adherence to effective medication to control it, a University of Otago study has found.
Lead author Dr. Simon Horsburgh, of the Department of Preventive and Social Medicine, says about 6 percent of adult New Zealanders have type 2 diabetes, with the figure much higher for Māori, Pacific peoples, Indo-Asians and people living in more socioeconomically deprived areas.
Metformin is the first-line pharmacological treatment for the disease in New Zealand. About 85 percent of people newly diagnosed with type 2 diabetes, who take medication for it, are prescribed the drug.
“It is an effective medication, but poor adherence has been linked to increased risk of complications and disease progression,” Dr. Horsburgh says.
The study, published in PLOS ONE, set out to describe the level of cycling between periods of adherence and non-adherence to metformin.
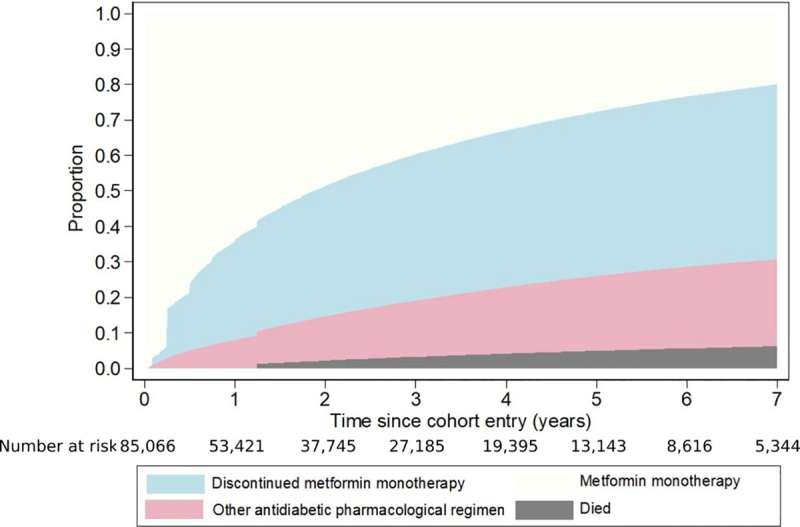
Researchers used Ministry of Health data of 85,000 people with type 2 diabetes to examine patterns of discontinuation (a gap of 90 or more days between the end of one metformin dispensing and the beginning of the next), and reinitiation of metformin use, between 2006 and 2014.
They found discontinuing metformin therapy was common, with 28 percent of the study members having discontinued at least once in the first year of treatment. This figure increased to 46 percent within five years of starting metformin.
However, of those people who did discontinue, 23 percent had reinitiated metformin within a year of their first discontinuation. This figure increased to 73 percent within five years of their first discontinuation.
More than half of the study members aged less than 35 years had discontinued metformin within a year of starting it. However, they were more likely to reinitiate metformin than older study members.
The ethnic groups most affected by type 2 diabetes—Māori, Pacific peoples and Indo-Asians—were more likely to discontinue metformin. However, they were also more likely to reinitiate after discontinuation.
“This points to metformin use being more cyclical in these groups, which is concerning—they will not be benefiting as much from the metformin as the periods of discontinuation are substantial. This will likely reduce its clinical effectiveness, potentially leading to these groups experiencing greater ill-health due to faster disease progression and increased type 2 diabetes complications,” Dr. Horsburgh says.
Also of concern was the finding of low adherence in younger age groups, as evidence is developing that people are developing type 2 diabetes at an earlier age.
He believes the study findings highlight the importance of interventions to improve use of metformin, not just at the individual and clinical consultation level, but also at the broader structural level of how health is delivered.
“Adherence is not just a patient characteristic or something that is solely under a person’s control. Health professionals need to be aware of how their services are provided and, in particular, how accessible they are to people from different backgrounds and with competing demands on their time and finances.
Source: Read Full Article