Study of severe COVID-19 helps uncover the roots of sepsis

Sepsis is a dreaded, life-threatening condition that can occur when an infection spins out of control. Like a tsunami after an earthquake, sepsis occurs when an infection triggers a dysregulation of the immune system, which leads to widespread organ damage and even death. The condition can result from nearly any kind of infection and afflicts tens of millions each year globally. Scientists don’t fully understand how it develops or how best to stop its progression in patients.
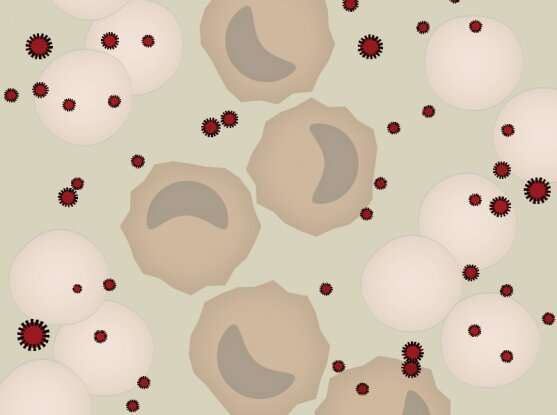
A new study by researchers at the Broad Institute of MIT and Harvard, Massachusetts General Hospital, and MIT offers new insight into what goes awry in the immune system during sepsis. By analyzing blood cells from COVID-19 patients who progressed to sepsis, they identified a cell type that impairs the body’s ability to detect and respond to the virus. The work helps explain how the immune system is suppressed in severe cases of COVID-19 and other infections, and suggests that targeting these cells could one day improve the outcome for patients. The study appears in Science Translational Medicine.
“Sepsis is a major problem around the world, and no one knows how to correct it,” said Nir Hacohen, co-senior author on the new study, institute member at the Broad, and director of the Mass General Center for Cancer Immunotherapy and Broad’s Cell Circuits Program. “The response to infection is complex, but work like this helps us to fill in the knowledge gaps and uncover new possibilities for treatment.”
In earlier work, the team analyzed individual immune cells in the blood of patients who had bacterial urinary tract infections, some of which resulted in sepsis. Patients with moderate urinary tract infections harbored a type of blood cell, dubbed MS1, which was even more abundant in septic patients. The MS1 cells were nearly absent from the blood of healthy control patients.
The researchers suspected that MS1 cells might also contribute to immune suppression during viral infections. By analyzing data collected earlier in the pandemic, the scientists observed higher abundance and activity of MS1 cells in severe cases of COVID-19 than in healthy controls.
To discover what drives the production of the cells, they added blood plasma from patients with sepsis or severe COVID-19 to healthy bone marrow cells in a dish, and found that this combination generated new MS1 cells. This indicated that some factors in the blood of severely infected patients—likely secreted immune molecules known as cytokines that were also identified in this study—drive the production of MS1 cells.
They next explored how MS1 cells alter the two main functions of the immune system: innate sensing of pathogens and the adaptive immune responses to them. The presence of MS1 cells generated from bone marrow prevented immune cells from sensing viral material. In addition, activated T immune cells divided more slowly in the presence of MS1 cells, indicating a more sluggish adaptive immune response to pathogens. The results suggest that MS1 cells strongly suppress the immune system in severe cases of COVID-19, sepsis, and many other infections.
“Studying cells in bulk can only get us so far. By analyzing individual cells from patients in carefully-designed clinical studies, and following up with functional studies, we can uncover unique cell types with big effects on physiology, such as the MS1 cells,” said co-senior author Paul Blainey, core member of the Broad and associate professor in the Department of Biological Engineering at MIT.
Source: Read Full Article