Study links post-COVID symptoms with alterations in gut microbiota

A team of scientists from Brazil has recently highlighted the significance of gut microbiota alterations induced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in triggering post-coronavirus disease 2019 (COVID-19) symptoms.
The study is currently available on the Research Square* preprint server.
Background
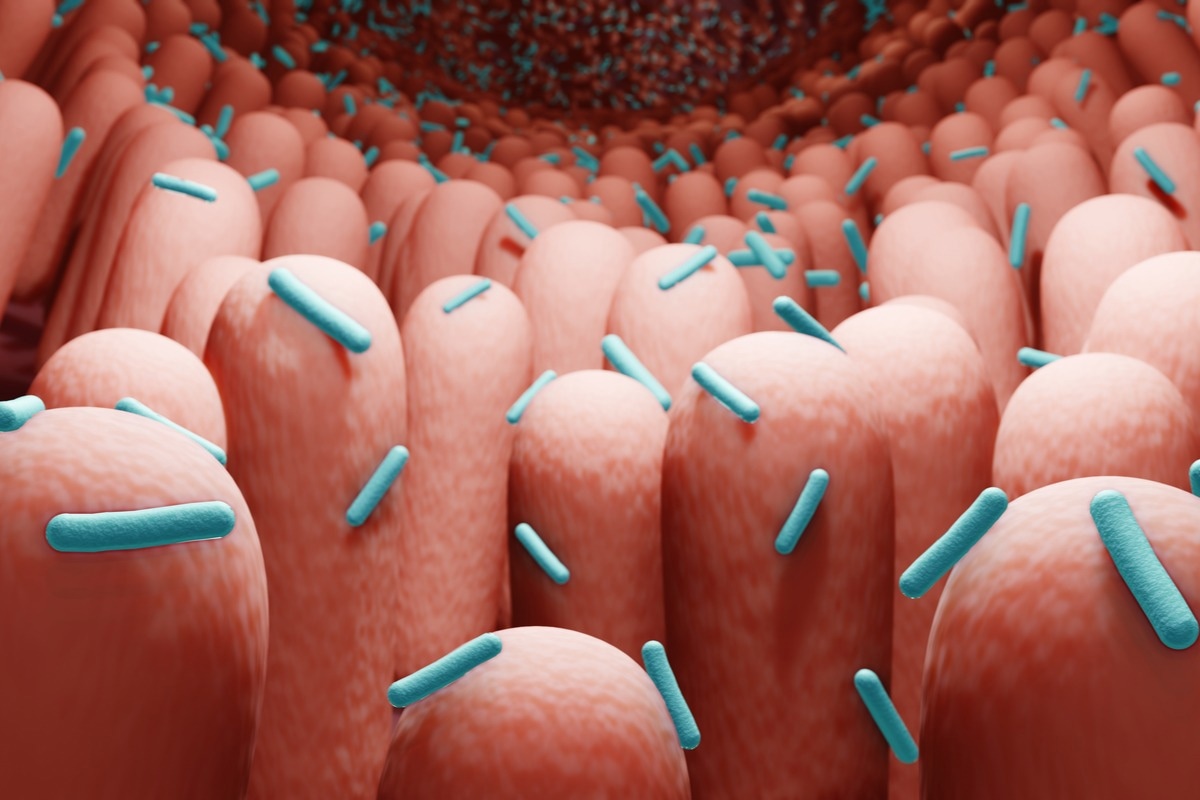
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of COVID-19, is known to infect a variety of organs beyond the respiratory tract. The most prominent one is the gastrointestinal tract infection, which causes considerable alteration in the gut microbiota composition and diversity. Studies conducted on COVID-19 patients have established an association between SARS-CoV-2-induced gut microbiota alteration and COVID-19 severity.
In the current study, the scientists have investigated the involvement of gut microbiota alteration in triggering post-COVID symptoms.
Study design
The study was conducted on a total of 72 post-COVID patients and 59 healthy individuals. The self-collected fecal samples were obtained from the participants for the analysis of gut microbiota composition and diversity. The samples from the COVID-19 patients were collected on average 2 months after SARS-CoV-2 infection. At the time of collection, all fecal samples tested negative for SARS-CoV-2.
To determine the functional role of SARS-CoV-2-altered gut microbiota in triggering post-COVID symptoms, the fecal samples collected from the participants were transplanted into germ-free mice.
Important observations
The analysis of fecal samples revealed no significant differences in the composition and diversity of gut microbiota between the COVID-19 patients and healthy individuals. However, the estimation of gut microbiota-derived metabolites in the samples revealed lower levels of acetate and butyrate in COVID-19 patients compared to that in healthy individuals. These findings indicate that SARS-CoV-2 infection alters the metabolism of gut microbiota.
Antimicrobial-resistant bacteria
To investigate the prevalence of antimicrobial-resistant bacteria in fecal samples, the Enterobacteriaceae family was selected for the analysis as these Gram-negative bacteria are known to transmit antimicrobial-resistance genes of clinical interest.
The findings revealed a significantly higher level of multidrug-resistant Enterobacteriaceae strains in the gut microbiota of COVID-19 patients compared to that in healthy individuals. A difference in the resistance to β-lactams and penicillin antibiotics was observed between COVID-19 patients and healthy individuals. In addition, an increased level of Klebsiella and a reduced level of antimicrobial-resistant Escherichia were observed in the gut microbiota of COVID-19 patients.
Intestinal homeostasis
Certain biomarkers of intestinal integrity and systemic inflammation were estimated to determine the impact of SARS-CoV-2 infection on overall intestinal homeostasis.
The findings revealed no significant difference in bacterial translocation from the gut between COVID-19 patients and healthy individuals. Similarly, no difference in blood levels of pro-inflammatory mediators was observed between the groups. However, a comparatively lower level of anti-inflammatory cytokine interleukin 10 (IL-10) and a higher level of intestinal epithelial damage were observed in COVID-19 patients.
Overall, these findings suggest that SARS-CoV-2 infection induces epithelial damage; however, it is not associated with higher systemic inflammation.
Post-COVID gut microbiome-induced changes in germ-free mice
The transplantation of post-COVID gut microbiota into the mice did not cause any significant alterations in the intestinal tract. However, the lung was identified as the most affected organ. Specifically, an increased level of lung inflammation was observed in mice that received gut microbiota of COVID-19 patients.
Importantly, no trace of SARS-CoV-2 RNA was detected in the lung tissues, which is in accordance with the absence of the virus in fecal samples. Thus, these findings confirm that the gut microbiota alteration due to viral infection can directly induce lung inflammation even in the absence of the virus.
Furthermore, the findings revealed that the transplantation of post-COVID gut microbiota can make the mice more susceptible to lung infection caused by the antimicrobial-resistant Klebsiella pneumoniae strain.
Regarding changes in the mice brain, decreased levels of neuroprotective factors, including brain-derived neurotrophic factor (BDNF) and postsynaptic density protein (PSD-95), and increased expression of tumor necrosis factor-alpha (TNF-alpha) was observed following post-COVID gut microbiota transplantation.
In addition, a significant impact of the post-COVID gut microbiota was observed on multiple biological pathways that are important for normal neurological functions. These changes were associated with a declined cognitive performance in mice.
For further confirmation, a mouse model of beta-coronavirus infection was used in the study. These mice also exhibited cognitive impairment due to viral infection.
The mice were first pre-treated with the probiotic bacteria Bifidobacterium longum 5 and subsequently subjected to coronavirus infection. The findings revealed that the probiotic-mediated modulation of the gut microbiota can prevent cognitive impairment associated with a viral infection.
Study significance
The study revealed that the gut microbiota alteration caused by SARS-CoV-2 infection could play a role in developing long-term COVID-19-related symptoms even after viral clearance.
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Viviani Mendes de Almeida. 2022. Gut microbiota from patients with mild COVID-19 cause alterations in mice that resemble post-COVID syndrome. Research Square. doi: https://doi.org/10.21203/rs.3.rs-1756189/v1 https://www.researchsquare.com/article/rs-1756189/v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Anti-Inflammatory, Bacteria, Blood, Brain, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, Gastrointestinal Tract, Genes, Inflammation, Interleukin, Metabolism, Metabolites, Microbiome, Mouse Model, Necrosis, Pathogen, Penicillin, Probiotic, Protein, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Tumor, Tumor Necrosis Factor, Virus

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article