Results of first clinical trial of niclosamide antiviral in patients with COVID-19 show further research needed

A clinical research team at Tufts Medical Center and Tufts University today published the results of the first randomized placebo-controlled clinical trial of the effectiveness of niclosamide, an oral medication long-used worldwide for treatment of tapeworms, in COVID-19 patients. The study, sponsored by Tufts Clinical and Translational Science Institute (CTSI) and funded by the National Institutes of Health (NIH), found that niclosamide did not show a statistically significant reduction in the percentage of adult outpatients with mild to moderate COVID-19 still testing positive at day three, but provided signals of benefit that warrant further study in larger trials.
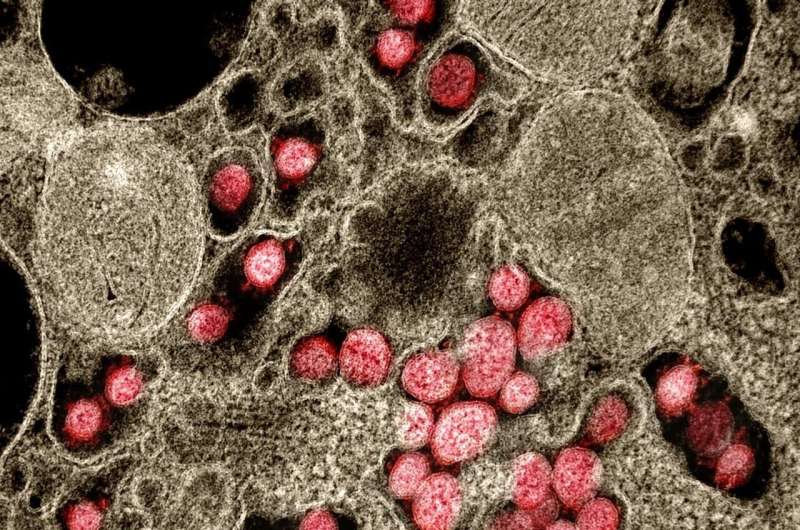
As reported today in JAMA Network Open, Principal Investigator Harry Selker, MD, MSPH, Dean of Tufts CTSI and Executive Director of the Institute for Clinical Research and Health Policy Studies at Tufts Medical Center, and colleagues, evaluated viral shedding of the virus that causes COVID-19, SARS-CoV-2. The study was conducted using an entirely remote clinical trial platform developed specifically for the study, to avoid requiring patients to have to visit the hospital and to support maintenance of participants’ self-quarantining.
Approved by the US FDA for treatment of tapeworm infection in 1982, and used worldwide for 50 years in millions of adults, pregnant women, and children as young as two years old, niclosamide is included in the World Health Organization (WHO) list of essential medicines, as it is very safe, and it is affordable and widely available. The researchers hypothesized that its antiviral characteristics seen in basic research experiments might prevent the COVID-19 SARS-CoV-2 virus from entering and replicating in human cells. Niclosamide has demonstrated antiviral efficacy across multiple variants of SARS-CoV-2 in laboratory studies, suggesting that it may be effective against COVID-19, including all variants of the virus.
The pre-selected time-point for testing niclosamide’s impact on oropharyngeal (respiratory) clearance of SARS-CoV-2 was at day three after treatment. At that point, a larger proportion of patients who took niclosamide were clear of the virus (66.7%) than those who received placebo (55.9%). However, with only 73 patients enrolled in the study, the difference was not statistically significant.
“With its long-standing excellent safety profile, worldwide availability, and promising antiviral activity, we are delighted to have been able to do the first study of niclosamide for treating COVID-19,” said Dr. Selker. “The patients who seemed to show the greatest benefit in terms of reducing contagious period and duration of symptoms were those with higher viral loads and likely more moderate disease. However, larger studies will be needed to further explore and confirm some of these promising signals, and potentially show niclosamide as a therapeutic option for preventing COVID-19-exposed individuals from even developing the disease.”
The study found that 45% of enrolled participants who shed SARS-CoV-2 via both oral and intestinal routes (i.e., present in stool) had higher viral loads than those with SARS-CoV-2 only detectable in oral swabs. Among those patients with higher overall viral load (and potentially moderate as opposed to mild disease), the average time to respiratory clearance of SARS-CoV-2 in the placebo group was 5.3 days, compared to 3.2 days in patients receiving niclosamide. However, in those patients with lower viral loads, the average time to clear SARS-CoV-2 from respiratory samples was faster, 2.9 days, regardless of treatment group.
Beyond the elimination of the virus from respiratory samples, the study looked at how long COVID-19 symptoms lasted. Across all patients, the average time to resolution of all symptoms was 14.6 days in the placebo group, compared to 12.0 days in the niclosamide group. This difference was greater in those patients with higher viral loads of SARS-CoV-2, with an average time to symptom resolution of 15.4 days in the placebo group, versus 10.5 days in the niclosamide group.
With obesity as a known risk factor for severe COVID-19, the average time to symptom resolution in participants with body mass indices (BMIs) of 25 or greater in the placebo arm was 16.5 days, compared to 11.6 days in the niclosamide group. These results indicate that niclosamide may reduce duration of COVID-related symptoms across higher-risk populations.
Niclosamide has been used worldwide for 50 years in millions of adults, pregnant women, and children as young as two years old. If it is proven to be effective for COVID-19, it will already be accepted as safe, and is already widely available. Also, it should not be affected by mutations in the SARS-CoV-2 virus.
The researchers plan additional, larger studies to determine the effectiveness of niclosamide in reducing the duration of COVID-19 contagiousness and symptoms in children and adolescents and pregnant women, and in preventing the disease in those who are exposed to COVID-19.
Source: Read Full Article