Patients with severe brachial plexus injuries who undergo amputation report benefits, study finds

Reconstruction surgery may not work for some people with severe brachial plexus injuries, so they choose to undergo amputation. In a retrospective review by Mayo Clinic researchers, these patients reported less mechanical shoulder pain, higher employment rates and more satisfaction after amputation. The paper appears online in the Journal of Bone & Joint Surgery.
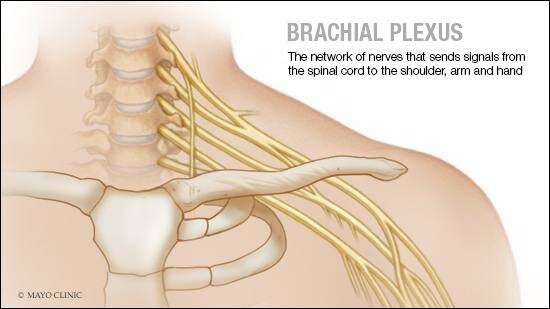
The brachial plexus is a network of nerves that sends signals from the spinal cord to the shoulder, arm and hand. The injury occurs when these nerves stretch, compress, rip apart or tear away from the spinal cord.
The most severe brachial plexus injuries usually result from motorcycle or car crashes. The injured person may lose feeling or movement in the shoulder, arm or hand, but surgery may help restore function. Surgical treatments include neurolysis (freeing up the nerve from scar tissue), nerve grafts and transfers, and muscle transfers. However, surgical reconstruction may not be feasible or work for some patients who seek amputation.
The authors performed 2,200 adult brachial plexus surgeries between June 2000 and June 2020. For this study, they reviewed records of the 32 patients who later underwent amputation. On average, the amputations took place about four years after the injury and 3½ years after the last reconstruction surgery. All patients had nerve and shoulder pain related to the weight of the injured arm.
Ten patients received myoelectric prostheses that use muscles in the remaining limb to control functions. Seventeen received traditional prostheses.
Researchers found that all the patients were likelier to be employed after amputation. All had less pain. None said they regretted undergoing amputation.
In addition, patients with myoelectric prostheses reported they used them regularly, compared with 29% of those with traditional prostheses. The patients with myoelectric prostheses also could grasp and release using the device. The authors say more research is needed to understand how the type of prostheses affects whether these patients use the device.
Source: Read Full Article