New technology tracks role of macrophages in cancer spread

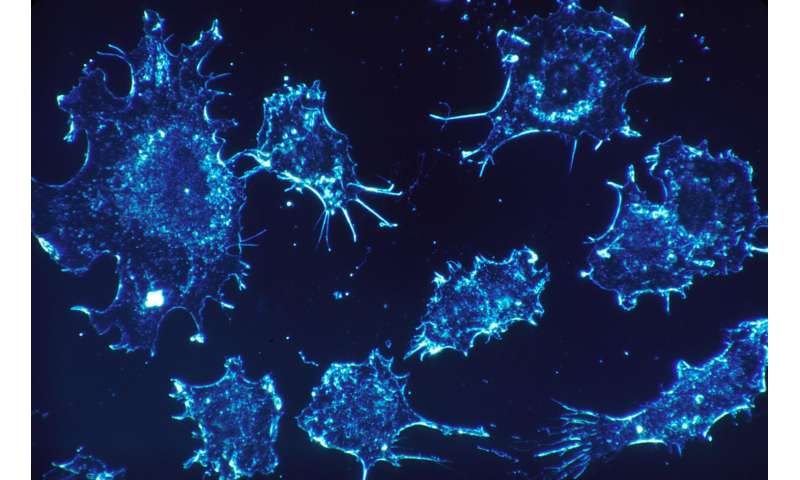
Macrophages, cells that help engulf and destroy harmful organisms in the body, tend to be characterized as the Jekyll and Hyde of the immune system.
Macrophages are essential first responders in fighting off infections and marshaling other immune cells to the scene. But they also play a major role in contributing to the growth and metastasis of many cancers, especially breast and pancreatic cancer.
New studies at the Morgridge Institute for Research paint a far less simple picture of macrophages, however. Rather than just “good” and “bad” populations, they find a surprisingly wide range of functionality, and better defining those differences may lead to more effective immunotherapies to fight cancer.
Writing this week in the journal Cancer Research, Morgridge researcher Tiffany Heaster and colleagues describe using a combination of technologies to better reveal macrophage function and behavior. The team applied fluorescence imaging to measure the precise metabolic activity of cells, then combined it with 3-D microfluidic technology allowing them to see, in real time, how the cells migrate and what role they play.
Importantly, the technologies helped them identify a distinct population of macrophage cells that migrate very actively toward cancer cells in their model—ones that may have outsized importance in promoting cancer growth. They used both mouse and human cells in the study and found comparable results, indicating this could be a powerful tool for examining the therapeutic potential of macrophages.
“There seems to be more of a spectrum of macrophage phenotypes, and it’s been really hard to get at what these phenotypes look like with standard measures,” says Heaster, who is now a senior researcher at Genentech after completing her Ph.D. in biomedical engineering at UW-Madison. “We really need to understand these better before we can target the bad macrophages and promote the good ones.”
Today, scientists classify two types of macrophages that operate in the tumor micro-environment, Heaster says. The first, called M1, actively kill cancer cells through methods such as piercing or eating the cells and stimulating secondary immune responses. The second, M2, actively support tumor growth by suppressing immune recognition and promoting blood vessel growth (angiogenesis).
They also appear to be a major culprit in metastasis. “There have been studies that have visualized how macrophages kind of latch on to each other and direct traffic (of cancer cells) toward the vasculature to escape,” she says.
Heaster says there is a very small subset of immunotherapies that target macrophages today, but they have limited uses compared to other immune cells, such as T cells, because they are poorly understood.
Heaster conducted the research in the lab of Melissa Skala, a Morgridge investigator and professor of biomedical engineering at UW-Madison. Skala says the key innovation is the convergence of two powerful technologies that give scientists a new way to study cancer. Skala is the lead developer of photonics-based technologies to develop personalized treatment plans for cancer. The microfluidics advances originated in the lab of Dave Beebe, a UW-Madison biomedical engineer and co-author on this project.
“Tiffany’s technology is helpful because it provides that single-cell resolution, and it provides spatial information so you can understand how different populations of macrophages are behaving metabolically, and how they’re distributed throughout the tumor,” Skala says.
Addressing macrophages with immunotherapy would help precisely because they are so diverse and may behave differently from one patient to the next, Skala says.
Source: Read Full Article