New technique ‘breaks the mold’ for 3D printing medical implants


Researchers have flipped traditional 3D printing to create some of the most intricate biomedical structures yet, advancing the development of new technologies for regrowing bones and tissue.
The emerging field of tissue engineering aims to harness the human body’s natural ability to heal itself, to rebuild bone and muscle lost to tumors or injuries.
A key focus for biomedical engineers has been the design and development of 3D printed scaffolds that can be implanted in the body to support cell regrowth.
But making these structures small and complex enough for cells to thrive remains a significant challenge.
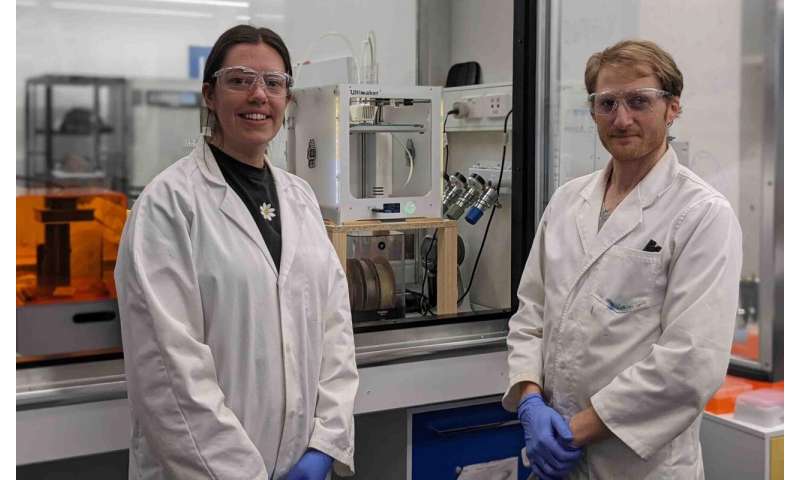
Enter a RMIT University-led research team, collaborating with clinicians at St Vincent’s Hospital Melbourne, Australia, who have overturned the conventional 3D printing approach.
Instead of making the bioscaffolds directly, the team 3D printed molds with intricately-patterned cavities then filled them with biocompatible materials, before dissolving the molds away.
Using the indirect approach, the team created fingernail-sized bioscaffolds full of elaborate structures that, until now, were considered impossible with standard 3D printers.
Lead researcher Dr. Cathal O’Connell said the new biofabrication method was cost-effective and easily scalable because it relied on widely available technology.
“The shapes you can make with a standard 3D printer are constrained by the size of the printing nozzle—the opening needs to be big enough to let material through and ultimately that influences how small you can print,” O’Connell, a Vice-Chancellor’s Postdoctoral Fellow at RMIT, said.
“But the gaps in between the printed material can be way smaller, and far more intricate.
“By flipping our thinking, we essentially draw the structure we want in the empty space inside our 3D printed mold. This allows us to create the tiny, complex microstructures where cells will flourish.”
Versatile technique
O’Connell said other approaches were able to create impressive structures, but only with precisely-tailored materials, tuned with particular additives or modified with special chemistry.
“Importantly, our technique is versatile enough to use medical grade materials off-the-shelf,” he said.
“It’s extraordinary to create such complex shapes using a basic ‘high school’ grade 3D printer.
“That really lowers the bar for entry into the field, and brings us a significant step closer to making tissue engineering a medical reality.”
The research, published in Advanced Materials Technologies, was conducted at BioFab3D@ACMD, a state-of-the-art bioengineering research, education and training hub located at St Vincent’s Hospital Melbourne.
Co-author Associate Professor Claudia Di Bella, an orthopedic surgeon at St Vincent’s Hospital Melbourne, said the study showcases the possibilities that open up when clinicians, engineers and biomedical scientists come together to address a clinical problem.
“A common problem faced by clinicians is the inability to access technological experimental solutions for the problems they face daily,” Di Bella said.
“While a clinician is the best professional to recognize a problem and think about potential solutions, biomedical engineers can turn that idea into reality.
“Learning how to speak a common language across engineering and medicine is often an initial barrier, but once this is overcome, the possibilities are endless.”
Future treatment toolkit
Currently there are few treatment options for people who lose a significant amount of bone or tissue due to illness or injury, making amputation or metal implants to fill a gap common outcomes.
While a few clinical trials of tissue engineering have been conducted around the world, key bioengineering challenges still need to be addressed for 3D bioprinting technology to become a standard part of a surgeon’s toolkit.
In orthopedics, a major sticking point is the development of a bioscaffold that works across both bone and cartilage.
“Our new method is so precise we’re creating specialized bone and cartilage-growing microstructures in a single bioscaffold,” O’Connell said.
“It’s the surgical ideal—one integrated scaffold that can support both types of cells, to better replicate the way the body works.”
Tests with human cells have shown bioscaffolds built using the new method are safe and non-toxic.
The next steps for the researchers will be testing designs to optimize cell regeneration and investigating the impact on cell regrowth of different combinations of biocompatible materials.
Step-by-step: How to reverse print a bioscaffold
The new method—which researchers have dubbed Negative Embodied Sacrificial Template 3D (NEST3D) printing—uses simple PVA glue as the basis for the 3D printed mold.
Once the biocompatible material injected into the mold has set, the entire structure is placed in water to dissolve the glue, leaving just the cell-nurturing bioscaffold.
Study first author, Ph.D. researcher Stephanie Doyle, said the method enabled researchers to rapidly test combinations of materials to identify those most effective for cell growth.
“The advantage of our advanced injection molding technique is its versatility,” Doyle said.
“We can produce dozens of trial bioscaffolds in a range of materials—from biodegradable polymers to hydrogels, silicones and ceramics—without the need for rigorous optimisation or specialist equipment.
“We’re able to produce 3D structures that can be just 200 microns across, the width of 4 human hairs, and with complexity that rivals that achievable by light-based fabrication techniques.
Source: Read Full Article