In Southeast Asia, robust immunity found up to 9 months after SARS-CoV-2 infection

In late December 2019, the World Health Organization (WHO) received a report of a cluster of severe pneumonia of unknown cause in Wuhan, China. Further investigation revealed that the causal agent was a novel betacoronavirus, namely, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Subsequently, SARS-CoV-2 caused the coronavirus disease 2019 (COVID-19) pandemic, whose clinical spectrum ranges from asymptomatic to mild upper respiratory illness to severe pneumonia resulting in death.
Background
After being infected with SARS-CoV-2, humans produce SARS-CoV-2-specific antibodies, memory B cells, and CD4+ and CD8+ T cells. All of these cells have well-defined functions in the elimination of the infection. The immune response mainly targets the structural proteins of a pathogen. In the case of SARS-CoV-2, targets of the immune response include the membrane protein (M), spike protein (S), and nucleoprotein (N).
The S protein consists of two domains (S1 and S2). The S1 region contains the receptor-binding domain (RBD) that interacts with the host’s angiotensin-converting enzyme 2 (ACE2), mediating viral entry. The RBD is a primary target of neutralizing antibodies. The S2 domain controls membrane fusion.
In addition to neutralization, antibodies activate various effector functions, which are mediated by their Fc domain. The persistence of serum antibodies may be one of the determinants of long-lasting immunity post-infection or vaccination. Anamnestic recall of memory T and B cells could also reduce infection at re-exposure as antibody titers decline. Memory immune response duration could depend on several factors, such as disease severity, cross-reactivity with human seasonal coronaviruses (hCoVs), ethnic background, age, etc.
Most studies on the evolution of the immune response to SARS-CoV-2 are conducted in Caucasian populations, partially due to a lack of data from high-risk areas. This lack of data from at-risk regions can hamper global vaccination efforts.
Now, a new study posted to the bioRxiv* preprint server focuses on functional immune memory to SARS-CoV-2, up to nine months in a Southeast Asian cohort, in the absence of re-infection.
A New Study
Sixty-four Cambodian individuals with confirmed SARS-CoV-2 infection were included in the initial study and re-assessed six to nine months later. The chances of re-infection were low as the incidence of COVID-19 was low in Cambodia during the follow-up period. In addition, 70% of the patients displayed mild or moderate symptoms, while 30% remained asymptomatic. Based on the duration of viremia, 53% were considered “long shedders” because of the detection of viral RNA for more than ten days.
Main Results
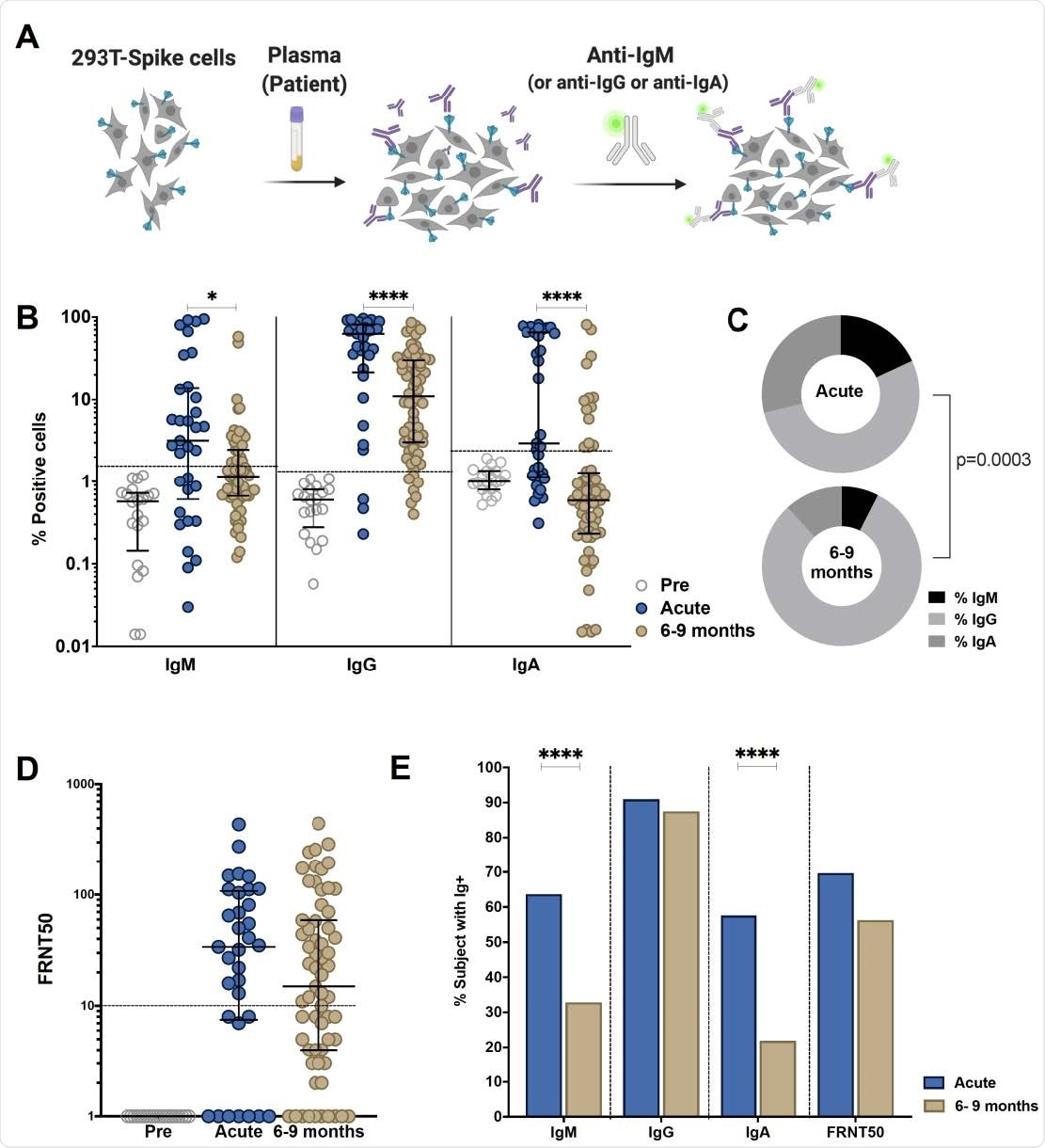
An S-Flow assay was used to test the presence of S-binding antibodies. Anti-S IgM, IgG, and IgA titers decreased significantly between the acute phase and late convalescence. The detection of neutralizing antibodies was achieved by foci reduction neutralization. Scientists observed no difference in the titers of neutralizing antibodies between the acute and convalescent phase, even though titers tended to decrease over time.
The frequency of individuals positive for anti-S IgG remained stable (88%), up to nine months post-infection. On the contrary, the frequency of individuals with neutralizing titers decreased to 56%. These findings showed that even though antibody titers decrease over time, the percentage of positive anti-S IgG individuals remains stable.
Between 55-66% of individuals showed antibody effector function activity up to nine months after infection. Scientists also found that S-, RBD- and N-specific memory B cells were maintained more than six months post symptom onset. Specifically, S1-and N- specific memory B cells persisted up to six to nine months post-infection, suggesting that B cells could be recruited after secondary exposure and might offer some protection against new variants.
Scientists also assessed anti-SARS-CoV-2 T cell immunity and observed the persistence of functional memory T cells, even after asymptomatic infection. Polyfunctional virus-specific CD4+ and CD8+ T cells were detected, mainly secreting IL-2 (16, 39). Virus-specific CD4+ and CD8+ cells could be detected in up to 90% and 70% of the individuals, respectively.
In this study, scientists observed no correlation between the S-specific cellular and humoral immune compartment at late convalescence. Moreover, correlations between anti-S antibody titers and Fc-related functions at late convalescence were found to be weak. Researchers concluded that serological testing alone might not be sufficient to understand the long-term immunity generated after SARS-CoV-2 infection completely.
Conclusion
The current study shows that different disease outcomes may have other implications for long-term immunity, influencing subsequent infection or vaccination.
Furthermore, this cohort study described the immune response in individuals of Asian origin and the absence of re-exposure to SARS-CoV-2. In addition, the scientists showed the persistence of humoral immunity, antibody effector functions, and virus-specific memory T and B cells six to nine months after infection. Therefore, this study enhances our understanding of long-term functional immunity.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Vo, T.M.H., et al. (2021) Robust and Functional Immunity up to 9 Months after SARS-CoV-2 Infection: A Southeast Asian Longitudinal. Cohort. doi: https://doi.org/10.1101/2021.08.12.455901, https://www.biorxiv.org/content/10.1101/2021.08.12.455901v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Assay, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, Enzyme, Evolution, Frequency, Immune Response, immunity, Laboratory, Membrane, Pandemic, Pathogen, Pneumonia, Protein, Receptor, Respiratory, Respiratory Illness, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article