I’m an asthmatic: What should I do during the coronavirus pandemic?


The new respiratory coronavirus COVID-19 is particularly worrying for the 2.7 million Australians who already suffer from asthma. That’s roughly one in nine people.
Viral respiratory infections, in particular those that cause the common cold, typically trigger flareups of asthma. They are the main reason for asthma episodes in both children and adults during autumn and winter.
So it’s natural for asthmatics to fear they may be more at risk during the coronavirus pandemic.
We don’t yet know if people with asthma are more susceptible to serious outcomes if they get COVID-19.
But there’s plenty asthmatics can do to minimize the impact of any viral infection, whether it’s the common cold or coronavirus.
Good asthma control
Asthma is characterized by inflammation in the lining of the lung’s air passages. For most asthmatic adults and some asthmatic children, the condition is long-term.
Asthmatic airway inflammation persists over time, even between acute attacks, and contributes significantly to day-to-day symptoms for some people.
If this airway inflammation is not treated, it can result in progressive narrowing of the airways. Normal lung function may never return.
Having “good asthma control” is the key starting point to reducing your risk.

That includes:
- having minimal or no day-to-day symptoms
- no night-time waking
- no asthma attacks and
- good lung function, such that you can do all your normal daily activities without any limitation.
Good asthma control is eminently achievable with regular medication (both relievers and preventers).
Relievers and preventers
Relievers are bronchodilators, meaning they act rapidly to relax the muscle in the airways and open the breathing passages to enable normal breathing.
Salbutamol (Ventolin or Asmol) is by far the best known and widely used, typically as an aerosol inhaler (often referred to as a puffer).
Preventers include Breo, Symbicort, Flutiform, Seretide and Flixotide.
The most commonly used preventer asthma medications in Australia contain an inhaled corticosteroid (which is anti-inflammatory) and a long-acting bronchodilator, which is a symptom controller—an ideal combination.
Proper preventer use may result in so few symptoms you might not need to take reliever medications for many weeks or even months.
People who are prescribed regular asthma preventer medications should continue to take them throughout the COVID-19 season to maximise their chances of staying well. Stopping these medications may increase the risk of having poorly controlled asthma and risk a severe attack or even hospital admission.
Stop panic-buying medications
Sadly, there has been a recent run on the reliever salbutamol in Australian pharmacies. While it’s vital people check the expiry date on their salbutamol canister, there is no need to stockpile these inhalers.
The less we panic-buy, the more likely there will be plenty of salbutamol available for those who need it.
Stay healthy, minimize the risk
To minimize your risk of a flare-up with any respiratory virus, including coronavirus, you should:
- take your preventer medication every day as prescribed
- make sure you know where your salbutamol inhaler is and that it hasn’t expired
- check in with your doctor to make sure your asthma control is as good as it can be, and that your current medications and doses are appropriate
- make sure you have an up to date written asthma action plan, and keep it handy
- remember to have your flu shot.
Written action plans mean you can step up your treatment if symptoms worsen. They provide guidance about when to start additional treatments such as a course of the anti-inflammatory corticosteroid prednisone or when to contact a doctor.
Your GP can help you recognise early symptoms of an asthma attack or flare-up, write a new plan and discuss the best way manage your attacks so you know exactly what to do if your symptoms increase.
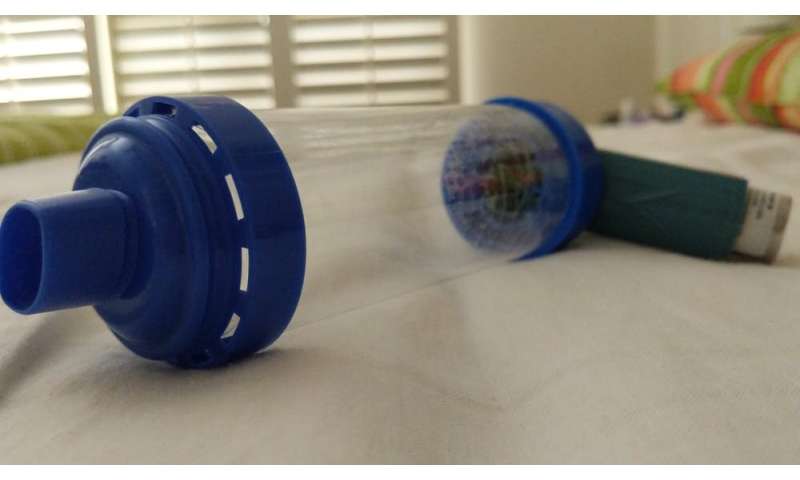
Your action plan should include advice to use a puffer and spacer during a flare-up of asthma, but not a nebuliser.
During the first SARS epidemic in 2003, health-care workers reportedly became ill due to exposure to aerosol-producing procedures such as nebulising bronchodilator medications.
We know that SARS CoV-2, the current pandemic virus, can spread rapidly this way and so nebulisers should not be used to treat asthma attacks at home or in hospital.
Good asthma control maximises the chances that if you do get coronavirus, it will have minimal impact. It doesn’t, however, remove the risk of a serious episode completely.
Patients, families and carers can get more information at Asthma Australia and health professionals can go to the National Asthma Council.
Source: Read Full Article